Aortic and Arterial Pulse Pressure
As the left ventricle ejects blood into the aorta, the aortic pressure increases to its peak systolic value. The greater the stroke volume, the greater the change in aortic pressure during ejection. The maximal change in aortic pressure during systole, from the time the aortic valve opens until the peak aortic pressure is attained (see Cardiac Cycle), represents the aortic pulse pressure, which is defined as the systolic pressure minus the diastolic pressure. For example, if the systolic pressure is 130 mmHg and the diastolic pressure is 85 mmHg, then the pulse pressure is 45 mmHg.
Pulse Pressure = Systolic Pressure − Diastolic Pressure
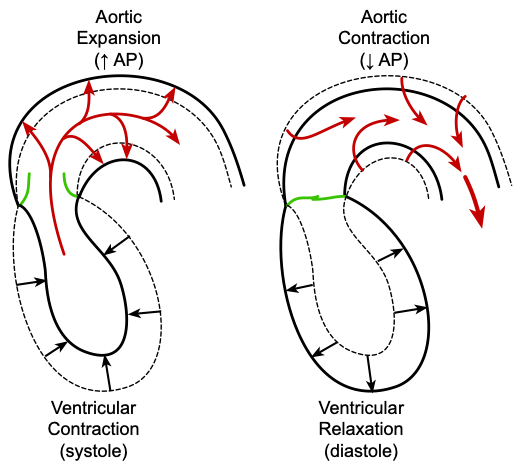 The rise in aortic pressure from its diastolic to systolic value is determined by the ventricular stroke volume and the compliance of the aorta. In the arterial system, the aorta has the highest compliance, due in part to a relatively greater proportion of elastin fibers versus smooth muscle and collagen. This serves the important function of dampening the pulsatile output of the left ventricle, reducing the pulse pressure (systolic minus diastolic arterial pressure). If the aorta were a rigid tube, the pulse pressure would be very high. Because the aorta is compliant, as the ventricle contracts and ejects blood into the aorta (red arrows on the left side of the figure), the walls of the aorta passively expand to accommodate the increase in blood volume. As the aorta expands in volume, the increase in pressure is determined by the compliance of the aorta for that range of volume change. As the blood leaves the aorta and the pressure falls, the walls of the aorta passively contract (recoil) until the next cardiac ejection (right side of the figure). At a given stroke volume, a less compliant (stiffer) aorta will have a greater pulse pressure because the systolic pressure will be higher and diastolic pressure will be lower (assuming unchanged systemic vascular resistance) because of greater elastic recoil during diastole. Therefore, aortic compliance and stroke volume are a major determinant of pulse pressure.
The rise in aortic pressure from its diastolic to systolic value is determined by the ventricular stroke volume and the compliance of the aorta. In the arterial system, the aorta has the highest compliance, due in part to a relatively greater proportion of elastin fibers versus smooth muscle and collagen. This serves the important function of dampening the pulsatile output of the left ventricle, reducing the pulse pressure (systolic minus diastolic arterial pressure). If the aorta were a rigid tube, the pulse pressure would be very high. Because the aorta is compliant, as the ventricle contracts and ejects blood into the aorta (red arrows on the left side of the figure), the walls of the aorta passively expand to accommodate the increase in blood volume. As the aorta expands in volume, the increase in pressure is determined by the compliance of the aorta for that range of volume change. As the blood leaves the aorta and the pressure falls, the walls of the aorta passively contract (recoil) until the next cardiac ejection (right side of the figure). At a given stroke volume, a less compliant (stiffer) aorta will have a greater pulse pressure because the systolic pressure will be higher and diastolic pressure will be lower (assuming unchanged systemic vascular resistance) because of greater elastic recoil during diastole. Therefore, aortic compliance and stroke volume are a major determinant of pulse pressure.
Summary:
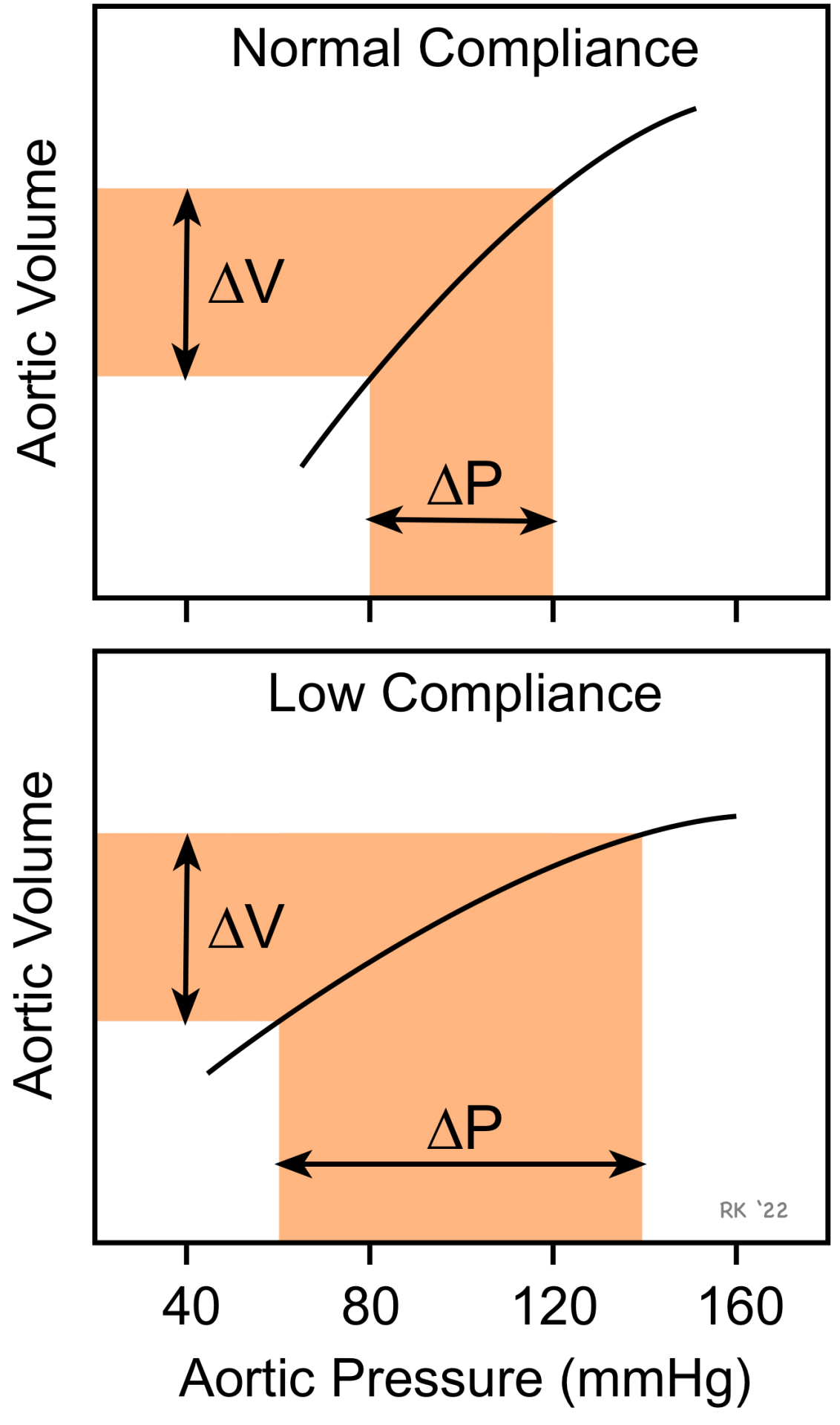 A highly compliant aorta (i.e., less stiff, normal aorta) has a smaller pulse pressure (ΔP) for a given stroke volume (ΔV) into the aorta than a stiff, low compliant aorta.
A highly compliant aorta (i.e., less stiff, normal aorta) has a smaller pulse pressure (ΔP) for a given stroke volume (ΔV) into the aorta than a stiff, low compliant aorta.- At elevated mean arterial pressures, compliance is decreased, which increases pulse pressure for a given stroke volume. This occurs because the compliance relationship in vessels is non-linear – i.e., it decreases at higher pressures.
- A larger stroke volume (not shown in the figure) produces a larger pulse pressure at any given compliance.
- Aortic compliance decreases with age and disease (e.g., arteriosclerosis) because of structural changes, producing increases in pulse pressure.
- At a given stroke volume, compliance determines pulse pressure, but not mean aortic pressure, which is determined by cardiac output and systemic vascular resistance.
- However, because vessels display dynamic compliance because of their viscoelastic behavior, increasing the rate of ventricular ejection (as occurs with increased ventricular inotropy) will increase the pulse pressure a small amount compared to the same volume ejected at a lower rate.
Revised 11/03/2023

 Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021)
Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021) Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)
Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)