Vascular Compliance
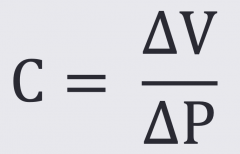 The ability of a blood vessel wall to expand and contract passively with changes in pressure is an important function of large arteries and veins. This ability of a vessel to distend and increase volume with increasing transmural pressure (inside minus outside pressure) is quantified as vessel compliance (C), which is the change in volume (ΔV) divided by the change in pressure (ΔP).
The ability of a blood vessel wall to expand and contract passively with changes in pressure is an important function of large arteries and veins. This ability of a vessel to distend and increase volume with increasing transmural pressure (inside minus outside pressure) is quantified as vessel compliance (C), which is the change in volume (ΔV) divided by the change in pressure (ΔP).
 The volume-pressure relationships (i.e., compliance) for an artery and vein are depicted in the figure. Two important characteristics stand out. First, the slope of the line, which represents the compliance at a given pressure, decreases as pressure increases because the blood vessel wall is a heterogeneous tissue comprising collagen, smooth muscle and elastin. Therefore, compliance decreases at higher pressures and volumes (i.e., vessels become "stiffer" at higher pressures and volumes). Second, at lower pressures (venous pressure is usually less than 15 mmHg), the compliance of a vein is about 10 to 20-times greater than an artery. Therefore, veins can accommodate a large change in blood volume with only a small change in pressure. The greater compliance of veins is largely the result of vein collapse that occurs at pressures less than 10 mmHg. At higher pressures and volumes, venous compliance (slope of compliance curve) is similar to arterial compliance. This characteristic makes veins suitable for use as arterial bypass grafts.
The volume-pressure relationships (i.e., compliance) for an artery and vein are depicted in the figure. Two important characteristics stand out. First, the slope of the line, which represents the compliance at a given pressure, decreases as pressure increases because the blood vessel wall is a heterogeneous tissue comprising collagen, smooth muscle and elastin. Therefore, compliance decreases at higher pressures and volumes (i.e., vessels become "stiffer" at higher pressures and volumes). Second, at lower pressures (venous pressure is usually less than 15 mmHg), the compliance of a vein is about 10 to 20-times greater than an artery. Therefore, veins can accommodate a large change in blood volume with only a small change in pressure. The greater compliance of veins is largely the result of vein collapse that occurs at pressures less than 10 mmHg. At higher pressures and volumes, venous compliance (slope of compliance curve) is similar to arterial compliance. This characteristic makes veins suitable for use as arterial bypass grafts.
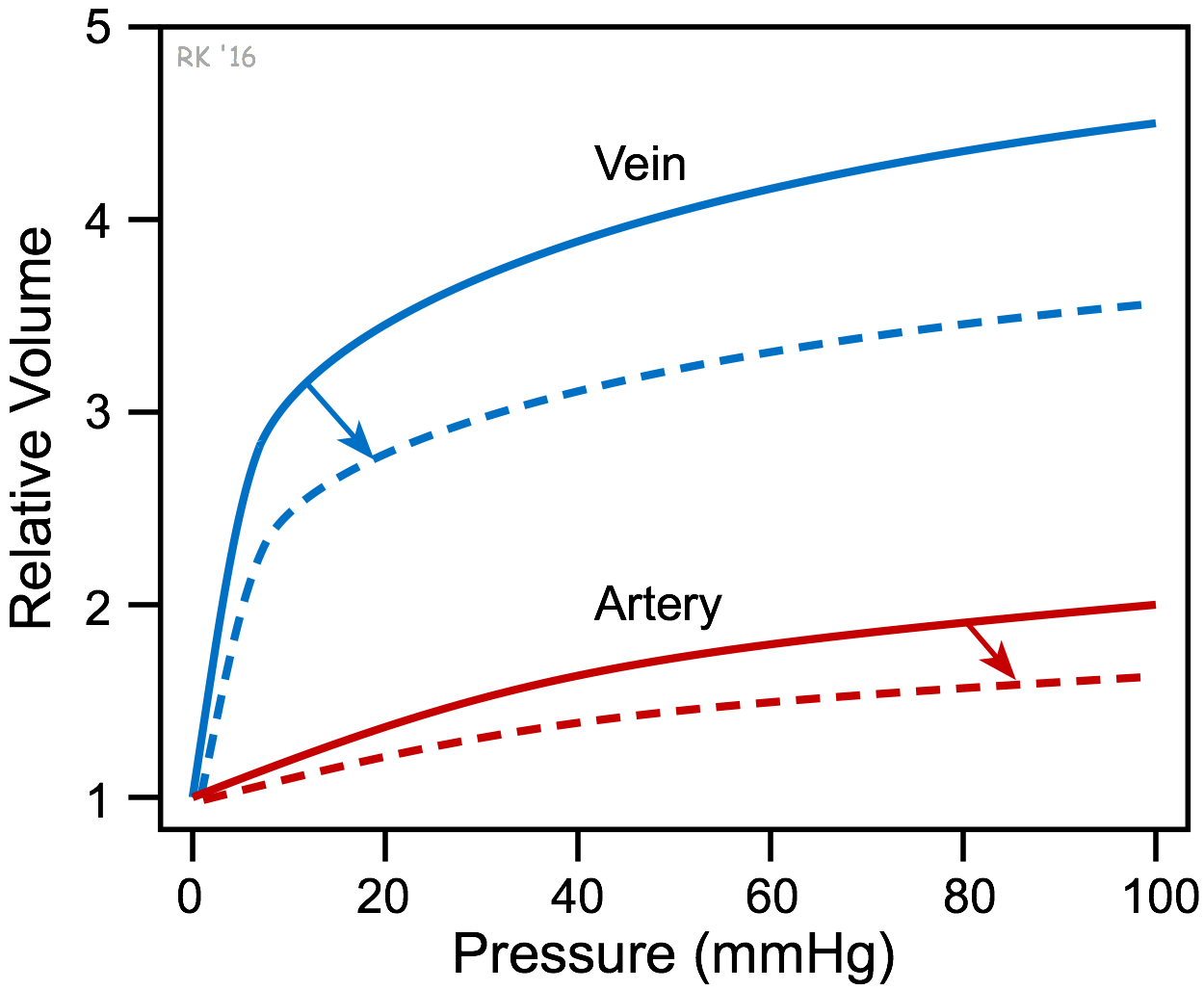 There is no single compliance curve for a blood vessel. For example, vascular smooth muscle contraction, which increases vascular tone, reduces vascular compliance (dashed lines in figure) and shifts the volume-pressure relationship downward. Conversely, smooth muscle relaxation increases compliance and shifts the compliance curve upward. This is important in the venous vasculature for regulating venous pressure and cardiac preload. Contraction of smooth muscle in arteries reduces their compliance, decreasing arterial blood volume and increasing arterial blood pressure within the arterial system. Another example of changing compliance is reduced aortic compliance with age or disease (e.g., arteriosclerosis). When this occurs, there is a qualitatively similar downward shift in the compliance curve for the aorta. Such compliance changes in the aorta are responsible for the increase in aortic pulse pressure with advanced age or arterial disease.
There is no single compliance curve for a blood vessel. For example, vascular smooth muscle contraction, which increases vascular tone, reduces vascular compliance (dashed lines in figure) and shifts the volume-pressure relationship downward. Conversely, smooth muscle relaxation increases compliance and shifts the compliance curve upward. This is important in the venous vasculature for regulating venous pressure and cardiac preload. Contraction of smooth muscle in arteries reduces their compliance, decreasing arterial blood volume and increasing arterial blood pressure within the arterial system. Another example of changing compliance is reduced aortic compliance with age or disease (e.g., arteriosclerosis). When this occurs, there is a qualitatively similar downward shift in the compliance curve for the aorta. Such compliance changes in the aorta are responsible for the increase in aortic pulse pressure with advanced age or arterial disease.
Compliance, as described above, represents the static compliance that is generated by expanding a vessel by a known volume and measuring the change in pressure at steady-state. However, before achieving a steady-state pressure, the pressure will actually be initially higher than the steady-state pressure when the volume of fluid is first added. The transient fall in pressure at a constant volume is called stress relaxation, and is related to the viscous properties of biological tissues. If the initial pressure increase is used instead of the steady-state pressure when the vessel volume is suddenly increased, the compliance will be lower (i.e., the vessel will appear stiffer). Therefore, the compliance of the vessel is also dependent upon the rate at which the change in volume occurs – i.e., there is a dynamic component to compliance.
Revised 12/8/2022

 Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021)
Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021) Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)
Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)