Reactive Hyperemia
 Reactive hyperemia is the transient increase in organ blood flow that occurs following a brief period of ischemia (e.g., arterial occlusion). Reactive hyperemia occurs following the removal of a tourniquet, unclamping an artery during surgery, or restoring flow to a coronary artery after recanalization (reopening a closed artery using an angioplasty balloon or clot-dissolving drug). The ability of an organ to display reactive hyperemia is related to its ability to display autoregulation.
Reactive hyperemia is the transient increase in organ blood flow that occurs following a brief period of ischemia (e.g., arterial occlusion). Reactive hyperemia occurs following the removal of a tourniquet, unclamping an artery during surgery, or restoring flow to a coronary artery after recanalization (reopening a closed artery using an angioplasty balloon or clot-dissolving drug). The ability of an organ to display reactive hyperemia is related to its ability to display autoregulation.
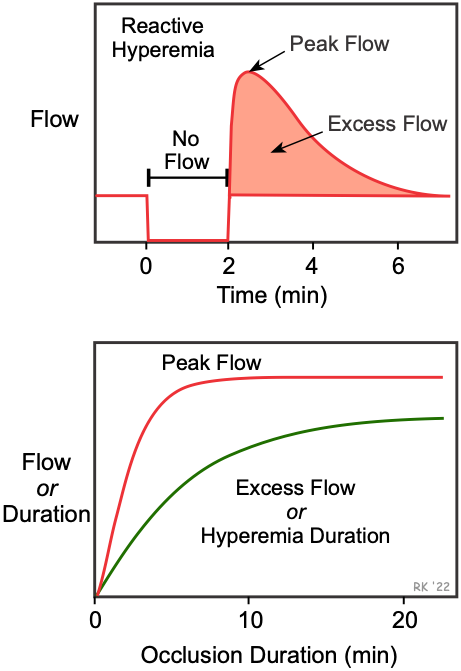
In the figure, the top panel shows the effects of a 2-minute arterial occlusion on blood flow. In this example, blood flow goes to zero during arterial occlusion. When the occlusion is released, blood flow rapidly increases (i.e., hyperemia occurs) that lasts for several minutes. Hyperemia occurs because during the period of occlusion, tissue hypoxia and a buildup of vasodilator metabolites dilate arterioles and decrease vascular resistance. Then, when perfusion pressure is restored (i.e., occlusion released), flow becomes elevated because of the reduced vascular resistance. During hyperemia, the tissue becomes reoxygenated and vasodilator metabolites are washed out of the tissue. This causes the resistance vessels to regain their normal vascular tone, returning flow to control. The longer the period of occlusion, the greater the metabolic stimulus for vasodilation, which leads to increases in peak reactive hyperemia, duration of hyperemia, and total excess flow. Depending upon the organ, maximal vasodilation (as indicated by peak flow), may occur following less than one minute (e.g., coronary circulation) of complete arterial occlusion, or may require several minutes of occlusion (gastrointestinal circulation). Myogenic mechanisms may also contribute to reactive hyperemia in some tissues. By this mechanism, arterial occlusion results in a decrease in pressure downstream in arterioles, which can lead to myogenic-mediated vasodilation.
Revised 11/03/2023

 Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021)
Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021) Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)
Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)