Autoregulation of Organ Blood Flow
Autoregulation is a manifestation of local blood flow regulation. It is defined as the intrinsic ability of an organ to maintain a constant blood flow despite changes in perfusion pressure. For example, if perfusion pressure is decreased to an organ (e.g., by partially occluding the arterial supply to the organ), blood flow initially falls, then partially returns to normal levels over the next few minutes. This autoregulatory response occurs in the absence of neural and hormonal influences and therefore is intrinsic to the organ, although these influences can modify the response. When perfusion pressure (arterial minus venous pressure, (PA - PV) initially decreases, blood flow (F) falls because of the following relationship between pressure, flow, and resistance:
When blood flow falls, arterial resistance (R) falls as the resistance vessels (small arteries and arterioles) dilate. Many studies suggest that metabolic, myogenic and endothelial mechanisms are responsible for this vasodilation. As resistance decreases, blood flow increases towards its normal value despite reduced perfusion pressure.
The figure below (left panel) shows the effects of suddenly reducing perfusion pressure from 100 to 70 mmHg. In a passive vascular bed that does not show autoregulation, this will cause a rapid and sustained fall in blood flow (black lines). In fact, the flow will fall more than the 30% fall in perfusion pressure because of passive diameter reduction as the intravascular pressure falls, which is represented by a slight increase in resistance in the passive vascular bed. If a vascular bed can undergo autoregulatory behavior, then after the initial fall in perfusion pressure and flow, the flow will gradually increase (red line) over the next few minutes as the vasculature dilates (resistance decreases – red line). After a few minutes, the flow will achieve a new steady-state level. If a vascular bed has a high degree of autoregulation (e.g., brain, coronary and renal circulations), then the new steady-state flow may be very close to normal despite the reduced perfusion pressure.
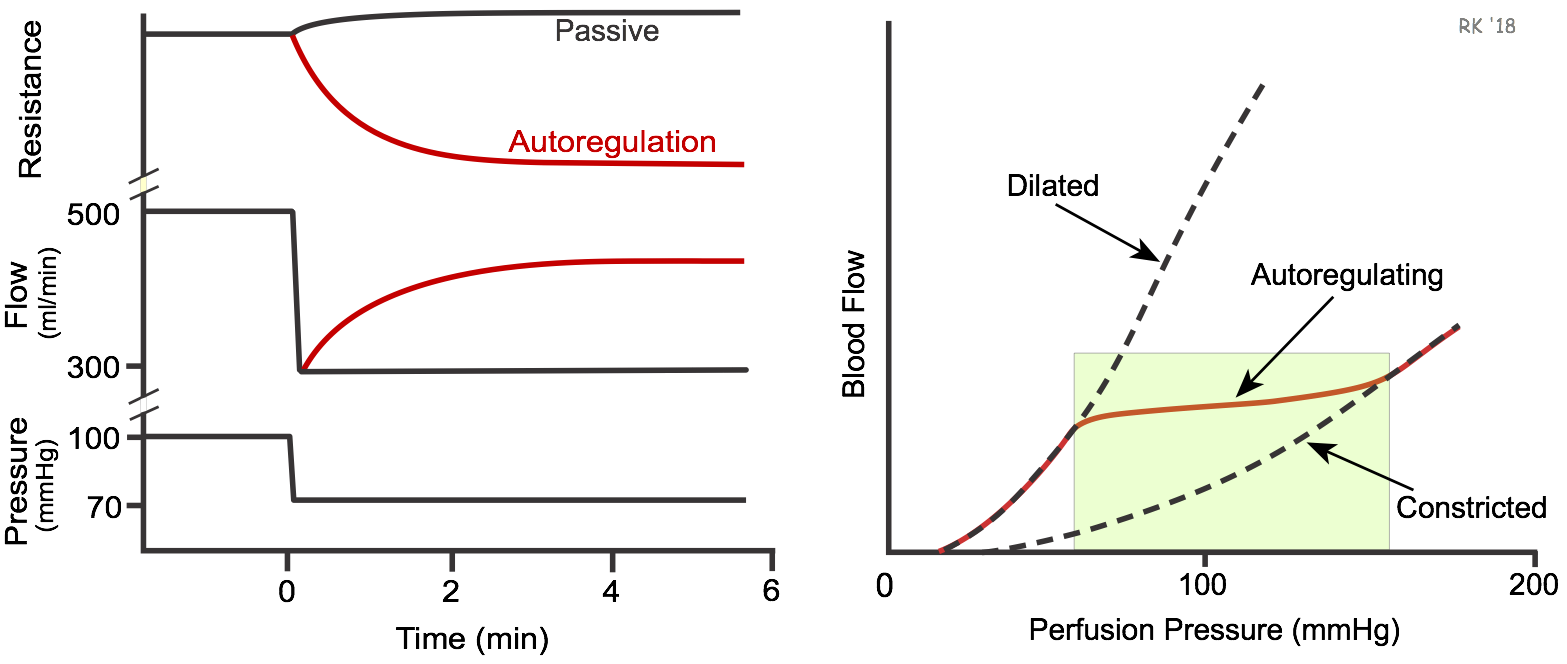
If an organ is subjected to an experimental study in which perfusion pressure is both increased and decreased over a wide range of pressures, and the steady-state autoregulatory flow response measured, then the relationship between steady-state flow and perfusion pressure can be plotted as shown in the above figure (right panel). The red line represents the autoregulatory responses in which flow changes relatively little, despite a large change in perfusion pressure. If a vasodilator drug is infused into an organ so that it is maximally dilated and incapable of autoregulatory behavior, the curve labeled "Dilated" is generated as perfusion pressure is changed. It is non-linear because blood vessels passively expand with increasing pressures, reducing resistance to flow. When the vasculature is not maximally dilated, many organs will display autoregulation as the perfusion pressure is reduced. When this occurs, there will be a range of perfusion pressures (i.e., autoregulatory range – green rectangle) in which flow may not decrease appreciably as perfusion pressure is reduced. The "Constricted" curve represents the pressure-flow relationship when the vasculature is maximally constricted and when autoregulation is not present. This figure also indicates that there is a pressure below which an organ is incapable of autoregulating its flow because it is maximally dilated. This perfusion pressure, depending upon the organ, may be between 50-70 mmHg. Below this perfusion pressure, blood flow decreases passively in response to further reductions in perfusion pressure. This has clinical implications in coronary, cerebral, and peripheral arterial disease, where proximal narrowing (stenosis) of vessels may reduce distal pressures below the autoregulatory range; hence, the distal vessels will be maximally dilated and further reductions in pressure will lead to reductions in flow. There is an upper limit to the autoregulatory range; however, this upper limit is seldom reached physiologically.
Different organs display varying degrees of autoregulatory behavior. The renal, cerebral, and coronary circulations show excellent autoregulation, whereas skeletal muscle and splanchnic circulations show moderate autoregulation. The cutaneous circulation shows little or no autoregulatory capacity.
Under what conditions does autoregulation occur, and why is it important? A change in systemic arterial pressure, as occurs for example with hypotension caused by hypovolemia or circulatory shock, can lead to autoregulatory responses in certain organs. In hypotension, despite baroreceptor reflexes that constrict much of the systemic vasculature, blood flow to the brain and myocardium does not decline appreciably (unless the arterial pressure falls below the autoregulatory range) because of the strong capacity of these organs to autoregulate. Autoregulation, therefore, ensures that these critical organs receive adequate blood flow and oxygen delivery.
There are situations in which systemic arterial pressure does not change, yet autoregulation is important. When a distributing artery to an organ becomes narrowed (e.g., atherosclerotic narrowing of lumen, vasospasm, or partial occlusion with a thrombus) this can cause an autoregulatory response. Narrowing (see stenosis) of distributing arteries increases their resistance and hence the fall in pressure along their length. This results in a reduced pressure distally within smaller arteries and arterioles, which are the primary vessels for regulating blood flow within an organ. These resistance vessels dilate in response to reduced pressure and blood flow. Autoregulation is indispensable in organs such as the brain and heart, in which partial occlusion of large arteries can lead to significant reductions in oxygen delivery, leading to tissue hypoxia and organ dysfunction.
Revised 11/03/2023

 Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021)
Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021) Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)
Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)