Redistribution of Vascular Pressures and Volumes
The following describes how changes in cardiac output and systemic vascular resistance alter the distribution of pressures and volumes within arterial and venous vasculature, assuming only passive changes in pressures and volumes. In the body, these passive changes are modified by various neural and hormonal reflexes, which are discussed under cardiac function and systemic vascular function curves. Also not included below are changes in cardiac output that rapidly occur in response to alterations in venous pressure (preload) and arterial pressure (afterload). Therefore, what is presented below serves as a model for understanding initial, passive cardiovascular changes that occur before being modified by intrinsic cardiac responses and extrinsic neurohumoral responses.
How Changes in Cardiac Output Affect Vascular Pressures and Volumes
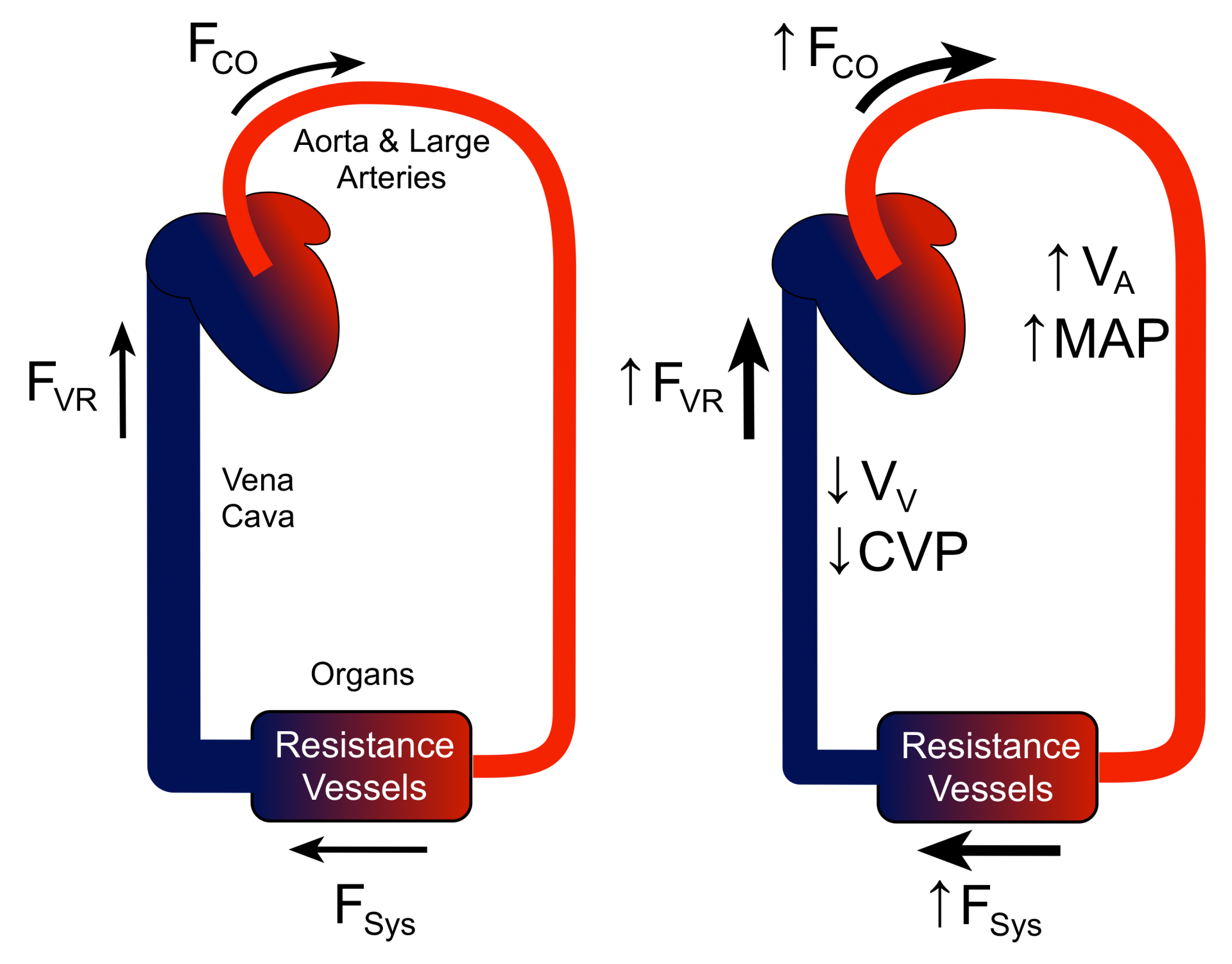 The blood volume contained within the aorta and large arteries, along with their compliance, determines the arterial pressure. Under steady-state conditions, the flow into the arterial system (FCO, cardiac output) equals the flow of blood from the large arteries into the organ vasculature (FSys, systemic flow). FSys equals the blood flow back into the heart (FVR, venous return). Therefore, FCO = FSys = FVR during steady-state conditions. Note that it is the resistance vessels within organs (small arteries and arterioles) that primarily determine the SVR. If FCO is suddenly increased without a change in SVR (right panel of figure), then the increased FCO into the large arteries will transiently be greater than FSys. This will cause arterial blood volume (VA) and mean arterial pressure (MAP) to increase. As the arterial pressure rises, FSyss increases until a new steady-state is reached where, once again, FCO = FSys (i.e., cardiac output and systemic flow are equally increased). In addition, because this is a closed system, FVR matches the other flows (FCO = FSys = FVR) in this new steady-state albeit at a higher arterial volume and pressure. Because the circulation is a closed system, the increase in arterial blood volume caused by the increase in cardiac output leads to a decrease in venous blood volume (VV), and therefore central venous pressure (CVP) decreases. If instead of increasing CO it is decreased, then the changes just described will be reversed; a decrease in CO causes arterial blood volume and pressure to decrease, and venous blood volume and pressure to increase. These shifts in pressure and volume are what happen, for example, when cardiac output is reduced in heart failure.
The blood volume contained within the aorta and large arteries, along with their compliance, determines the arterial pressure. Under steady-state conditions, the flow into the arterial system (FCO, cardiac output) equals the flow of blood from the large arteries into the organ vasculature (FSys, systemic flow). FSys equals the blood flow back into the heart (FVR, venous return). Therefore, FCO = FSys = FVR during steady-state conditions. Note that it is the resistance vessels within organs (small arteries and arterioles) that primarily determine the SVR. If FCO is suddenly increased without a change in SVR (right panel of figure), then the increased FCO into the large arteries will transiently be greater than FSys. This will cause arterial blood volume (VA) and mean arterial pressure (MAP) to increase. As the arterial pressure rises, FSyss increases until a new steady-state is reached where, once again, FCO = FSys (i.e., cardiac output and systemic flow are equally increased). In addition, because this is a closed system, FVR matches the other flows (FCO = FSys = FVR) in this new steady-state albeit at a higher arterial volume and pressure. Because the circulation is a closed system, the increase in arterial blood volume caused by the increase in cardiac output leads to a decrease in venous blood volume (VV), and therefore central venous pressure (CVP) decreases. If instead of increasing CO it is decreased, then the changes just described will be reversed; a decrease in CO causes arterial blood volume and pressure to decrease, and venous blood volume and pressure to increase. These shifts in pressure and volume are what happen, for example, when cardiac output is reduced in heart failure.
How Changes in Systemic Vascular Resistance Affect Vascular Pressures and Volumes
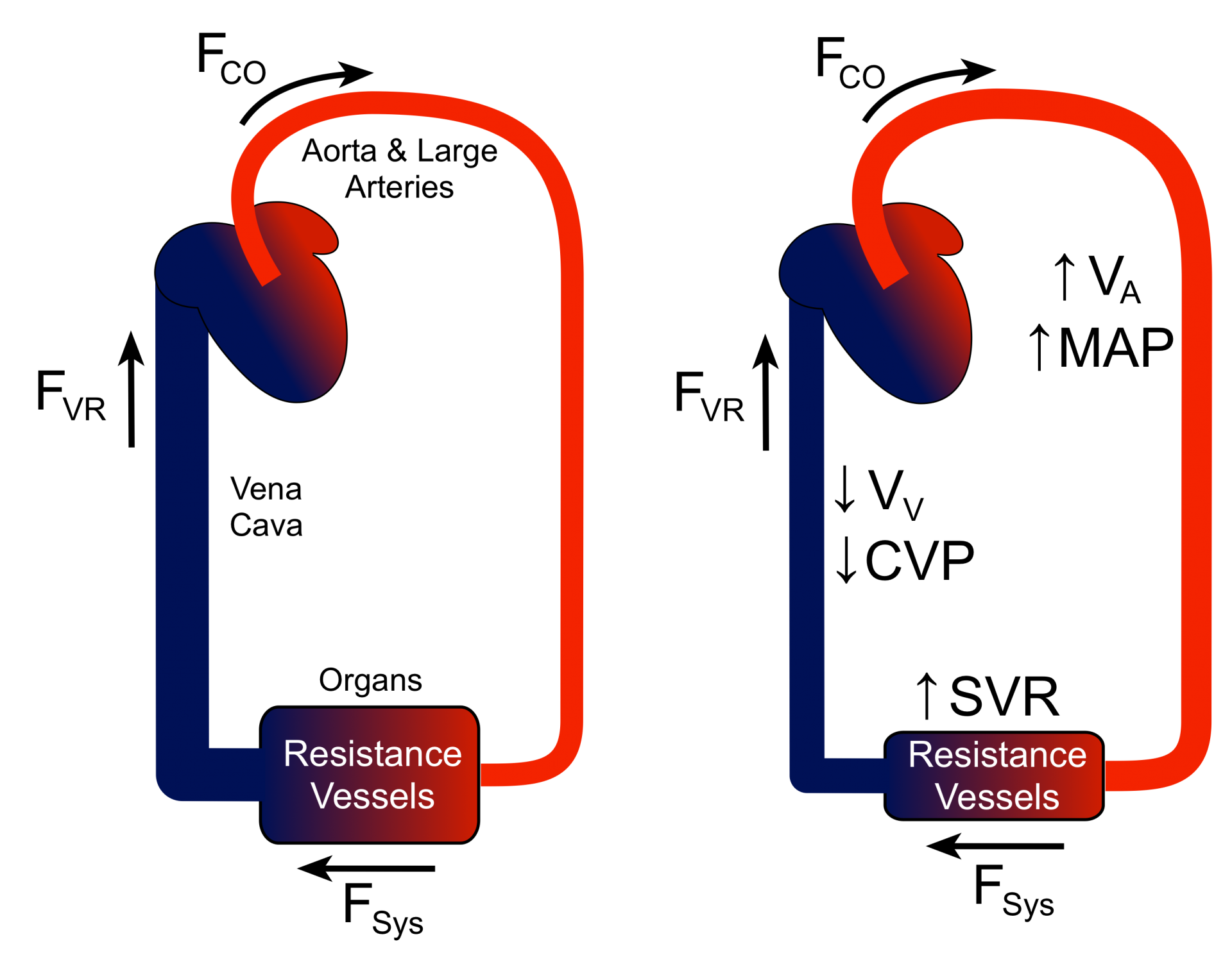 The figure shows how increasing SVR (right panel) without changing CO affects vascular volumes and pressures. If organ resistance vessels constrict, organ vascular resistance increases, which increases SVR. This transiently reduces FSys, which when coupled with a constant flow into the large arteries (FCO), causes the blood volume and pressure within the arterial system to increase (right panel). As the arterial pressure increases, FSys increases despite the increased resistance until organ blood flow once again equals the flow into the arterial system (FCO = FSys). In this new steady-state condition, the blood volume and pressure within the large arteries will be increased, causing FSys and FVR to once again be equal to FCO. As with the increase in CO at constant SVR, the increase in arterial blood volume and pressure causes a reciprocal reduction in venous blood volume and pressure. If SVR is decreased instead of increased, then the changes described above will be the opposite. A decrease in SVR causes arterial blood volume and pressure to decrease because FSys is transiently greater than FCO, which causes venous blood volume and pressure to increase. This happens in the body when an arterial vasodilator drug is given to treat high blood pressure; however, the pressure lowering effect of the drug is partially counteracted by an increase in FCO caused by baroreceptor reflexes and by reduced arterial pressure (afterload), which increases left ventricular stroke volume.
The figure shows how increasing SVR (right panel) without changing CO affects vascular volumes and pressures. If organ resistance vessels constrict, organ vascular resistance increases, which increases SVR. This transiently reduces FSys, which when coupled with a constant flow into the large arteries (FCO), causes the blood volume and pressure within the arterial system to increase (right panel). As the arterial pressure increases, FSys increases despite the increased resistance until organ blood flow once again equals the flow into the arterial system (FCO = FSys). In this new steady-state condition, the blood volume and pressure within the large arteries will be increased, causing FSys and FVR to once again be equal to FCO. As with the increase in CO at constant SVR, the increase in arterial blood volume and pressure causes a reciprocal reduction in venous blood volume and pressure. If SVR is decreased instead of increased, then the changes described above will be the opposite. A decrease in SVR causes arterial blood volume and pressure to decrease because FSys is transiently greater than FCO, which causes venous blood volume and pressure to increase. This happens in the body when an arterial vasodilator drug is given to treat high blood pressure; however, the pressure lowering effect of the drug is partially counteracted by an increase in FCO caused by baroreceptor reflexes and by reduced arterial pressure (afterload), which increases left ventricular stroke volume.
Revised 11/03/2023

 Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021)
Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021) Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)
Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)