Tissue Edema and General Principles of Transcapillary Fluid Exchange
Edema refers to the swelling of a tissue that results from excessive accumulation of fluid within the tissue. Edema can be highly localized, for example, to a small region of the skin subjected to a bee sting. Edema, however, can also comprise an entire limb, specific organs such as the lungs (e.g., pulmonary edema) or the whole body.
General principles
A 38-minute lecture on this topic (including linked pages) can be viewed by clicking on Capillary Fluid Exchange.
To understand how edema occurs, it is first necessary to explain the concept of tissue compartments. There are two primary fluid compartments in the body between which fluid is exchanged – the intravascular and extravascular compartments. The intravascular compartment contains fluid (i.e., blood) within the cardiac chambers and the vascular system of the body. The extravascular system is everything outside the intravascular compartment. Fluid and electrolytes readily move between these two compartments. The extravascular compartment comprises many subcompartments, such as the cellular, interstitial, and lymphatic subcompartments, and a specialized system containing cerebrospinal fluid in the central nervous system.
The movement of fluid and accompanying solutes between compartments (mostly water, electrolytes, and small molecular weight solutes) is governed by physical factors such as hydrostatic and oncotic forces. These forces are normally balanced in such a manner that fluid volume remains relatively constant between the compartments. If the physical forces or barriers to fluid movement are altered, the volume of fluid may increase in one compartment and decrease in another. Sometimes, total fluid volume increases in the body so that both intravascular and extravascular compartments increase in volume. This can occur, for example, when the kidneys cannot excrete sufficient amounts of sodium and water.
When the fluid volume within the interstitial compartment (space between the cells and blood vessels) increases, this compartment increases in size, leading to tissue swelling (i.e., edema). This happens, for example, when an ankle is sprained and swells. When excess fluid accumulates within the peritoneal space (space between the abdominal wall and organs), this is termed "ascites." Pulmonary congestion, which can occur in heart failure as the left atrial pressure increases and blood backs up in the pulmonary circuit, causes pulmonary edema.
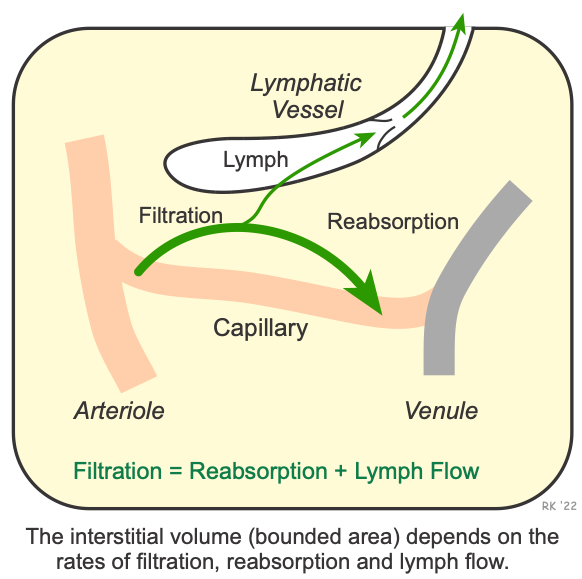 A model that helps us to understand what causes edema is shown to the right. Filtration is the movement of fluid out of the capillary, and reabsorption is the movement of fluid back into the capillary. In most capillary systems of the body, there is a small net filtration (typically about 1% of plasma) of fluid from the intravascular to the extravascular compartment. Capillary fluid filtration exceeds reabsorption. This would cause fluid to accumulate within the interstitium (i.e., cause edema) over time if it were not for the lymphatic system that removes excess fluid from the interstitium and returns it back into the intravascular compartment. Therefore, fluid balance occurs when:
A model that helps us to understand what causes edema is shown to the right. Filtration is the movement of fluid out of the capillary, and reabsorption is the movement of fluid back into the capillary. In most capillary systems of the body, there is a small net filtration (typically about 1% of plasma) of fluid from the intravascular to the extravascular compartment. Capillary fluid filtration exceeds reabsorption. This would cause fluid to accumulate within the interstitium (i.e., cause edema) over time if it were not for the lymphatic system that removes excess fluid from the interstitium and returns it back into the intravascular compartment. Therefore, fluid balance occurs when:
Filtration = Reabsorption + Lymphatic Flow
Circumstances, however, can arise in which net capillary filtration exceeds the capacity of the lymphatics to carry away the fluid (i.e., net filtration > lymph flow). When this occurs, the interstitium swells with fluid, becoming edematous.
Factors Precipitating Edema
- Increased capillary hydrostatic pressure (as occurs when venous pressures become elevated by gravitational forces, in heart failure, or with venous obstruction)
- Decreased plasma oncotic pressure (as occurs with hypoproteinemia during malnutrition)
- Increased capillary permeability caused by proinflammatory mediators (e.g., histamine, bradykinin) or by damage to the structural integrity of capillaries so that they become "leakier" (as occurs in tissue trauma, burns, and severe inflammation)
- Lymphatic obstruction (as occurs in filariasis or with tissue injury)
Prevention and Treatment of Edema
The treatment for edema involves altering one or more of the physical factors that regulate fluid movement. For example, in edema (pulmonary or systemic) secondary to heart failure, diuretic drugs are given to reduce blood volume and venous pressure. In heart failure patients, improving cardiac output by using cardiostimulatory or vasodilator drugs reduces venous and capillary pressures, decreasing filtration and promoting reabsorption of fluid within tissues (click here to see why increasing cardiac output decreases venous pressure). If a patient suffers from ankle edema, that person will be instructed to keep their feet elevated (to diminish the effects of gravity on capillary pressure), use tight-fitting elastic stockings (to increase tissue hydrostatic pressure), and possibly be prescribed a diuretic drug to enhance fluid removal by the kidneys.
Revised 11/05/2023
 Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021)
Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021) Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)
Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)