Angina
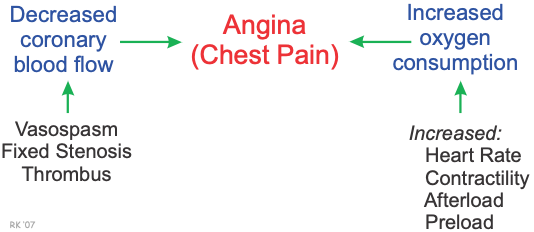 Angina is chest pain or discomfort caused by an imbalance between oxygen supply (decreased coronary blood flow) and oxygen demand (increased myocardial oxygen consumption), which leads to a decrease in the oxygen supply/demand ratio and myocardial hypoxia. The decreased flow can result from coronary artery vasospasm, fixed stenotic lesions (chronic vessel narrowing), or from a blood clot (thrombus) that incompletely (non-occlusive thrombus) or completely occludes a coronary artery (occlusive thrombus). Oxygen consumption can be elevated by increased heart rate, contractility (inotropy), afterload and preload.
Angina is chest pain or discomfort caused by an imbalance between oxygen supply (decreased coronary blood flow) and oxygen demand (increased myocardial oxygen consumption), which leads to a decrease in the oxygen supply/demand ratio and myocardial hypoxia. The decreased flow can result from coronary artery vasospasm, fixed stenotic lesions (chronic vessel narrowing), or from a blood clot (thrombus) that incompletely (non-occlusive thrombus) or completely occludes a coronary artery (occlusive thrombus). Oxygen consumption can be elevated by increased heart rate, contractility (inotropy), afterload and preload.
Types of Angina
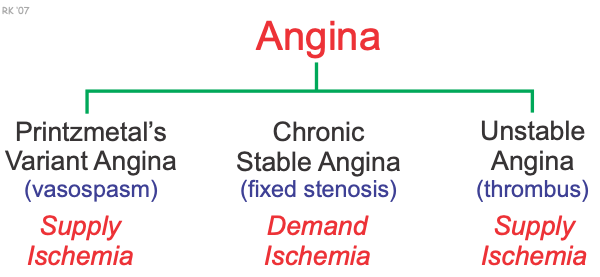
There are three types of angina: Printzmetal's variant angina, chronic stable angina, and unstable angina. All three forms are associated with a reduction in the oxygen supply/demand ratio.
Variant (Printzmetal's) Angina
Variant (Printzmetal's) angina results from coronary vasospasm, which temporarily reduces coronary blood flow. This produces ischemia by reducing the oxygen supply ("supply ischemia"), thereby decreasing the oxygen supply/demand ratio. Enhanced sympathetic activity (e.g., during emotional stress), especially when coupled with a dysfunctional coronary vascular endothelium (i.e., reduced endothelial production of the vasodilators nitric oxide and prostacyclin) can precipitate vasospastic angina. This form of angina is treated with drugs that reverse or inhibit coronary vasospasm. These drugs include calcium-channel blockers and nitrodilators. These drugs also reduce oxygen demand to further improve the oxygen supply/demand ratio.
Chronic Stable Angina
Chronic stable angina is caused by a chronic narrowing (stenosis) of coronary arteries due to atherosclerosis. Coronary stenosis is readily observed in the large epicardial arteries by angiography and other imaging techniques; however, narrowing also occurs in smaller branches that cannot be visualized angiographically. When a coronary artery narrows beyond a critical value (critical stenosis), the myocardial tissue perfused by the artery will not receive adequate blood flow because coronary flow reserve (i.e., maximal flow capacity) decreases. This results in the tissue becoming ischemic and hypoxic, particularly during times of increased oxygen demand (e.g., during physical exertion). Therefore, in this type of angina, relative ischemia occurs when the oxygen demand increases, so this is referred to as "demand ischemia." This leads to angina during physical exertion (exertional angina). The discomfort is usually associated with a predictable threshold of physical activity. Other conditions that cause myocardial oxygen demand to increase, such as a large meal or emotional stress, can also precipitate pain. This form of angina is most commonly treated with drugs that reduce oxygen demand. These drugs include beta-blockers, calcium-channel blockers, nitrodilators. They act by decreasing heart rate, contractility, afterload and preload.
Unstable Angina
Unstable angina is caused by transient formation and dissolution of a blood clot (thrombosis) within a coronary artery. The clots often form in response to plaque rupture in atherosclerotic coronary arteries; however, the clot may also form because diseased coronary artery endothelium (endothelial dysfunction) is unable to produce nitric oxide and prostacyclin that inhibit platelet aggregation and clot formation. When the clot forms, coronary flow is reduced, leading to a reduction in the oxygen supply/demand ratio ("supply ischemia"). If the clot completely occludes the coronary artery for a sufficient period of time, the myocardium supplied by the vessel may become infarcted (acute myocardial infarction) and become irreversibly damaged. Unstable angina is treated with drugs that reduce oxygen demand (i.e., beta-blockers, calcium-channel blockers, nitrodilators), but more importantly, this form of angina is treated with drugs that inhibit thrombus formation (e.g., antiplatelet drugs and aspirin).
Angina may also be precipitated by a combination of supply and demand ischemia. For example, diseased, stenotic coronary segments can sometimes undergo vasoconstriction during exercise (healthy arteries dilate). This probably occurs because of the absence of sufficient production of nitric oxide and perhaps prostacyclin by the vascular endothelium to counteract normal sympathetic-mediated effects on vascular alpha-adrenoceptors.
A hemodynamic condition may exist that leads to coronary vascular steal. In this condition, multiple fixed stenotic lesions can lead to a redistribution of flow within the major supply arteries of the heart under conditions of exercise or vasodilator therapy. As blood flow increases in one region of the coronary vascular network, blood flow can reciprocally decrease in another region, leading to angina.
Revised 01/29/2023

 Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021)
Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021) Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)
Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)