Vascular Steal
The presence of stenotic lesions in multiple arteries can lead to a condition called "vascular steal." This occurs when dilation of one vascular network (e.g., during exercise or vasodilator therapy) "steals" blood flow from another region within the organ that is already maximally dilated because of the presence of proximal lesions.
Vascular steal can occur in the coronary vasculature, in the lower limb vasculature, or in any vascular network when specific conditions are met. The model described below is for the coronary vasculature.
Conditions:
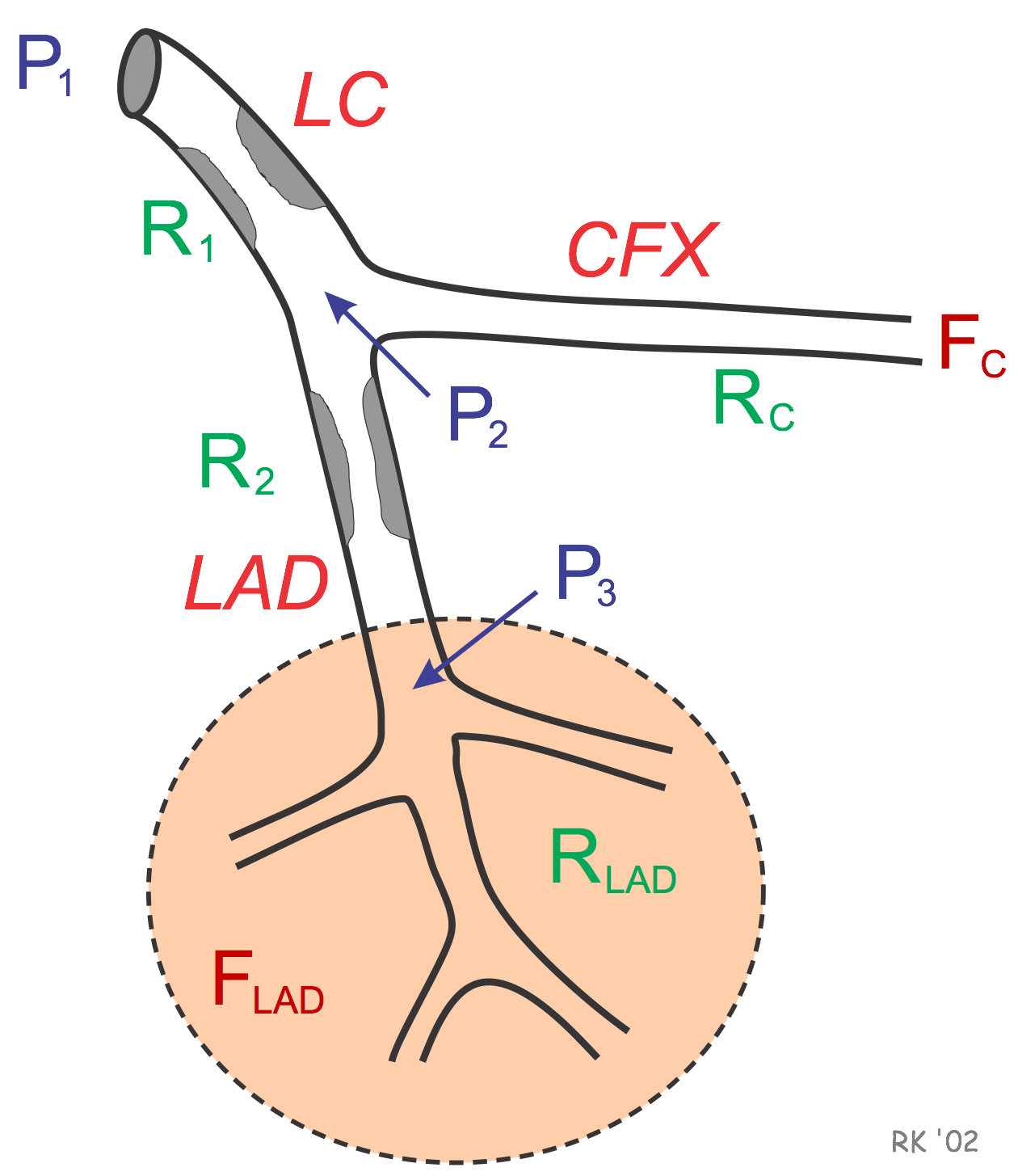 Clinically significant lesions in left main coronary artery (LC) and left anterior descending artery (LAD), R1 and R2, respectively.
Clinically significant lesions in left main coronary artery (LC) and left anterior descending artery (LAD), R1 and R2, respectively.- The pressure distal to the LAD lesion (P3) divided by resistance of the vasculature supplied by the LAD (RLAD) determines blood flow in the LAD-supplied distal vascular beds (FLAD). The vascular bed supplied by the LAD is maximally dilated (i.e., at minimal resistance, RLAD) because of autoregulation in response to the large reduction in pressure distal to the LAD lesion (P3) caused by the combined LC and LAD stenotic lesions (R1 and R2, respectively).
- Blood flow in the circumflex (CFX)-supplied vascular beds (FC) is determined by P2 divided by the resistance of the distal vascular beds supplied by the circumflex artery (RC). If the LC lesion does not reduce P2 to a value below the autoregulatory range of the CFX-supplied vascular beds, then these beds will not be maximally dilated and therefore can still decrease their resistance (RC) in response to increased metabolic demand by the heart or to vasodilator drugs.
In the above example, vasodilator stimuli (e.g., exercise or drugs) will decrease RC and increase FC. When this increase in CFX blood flow occurs, the increased flow across R1 supplying the increase in FC will further decrease P2 because the pressure gradient across R1 (P1 - P2) is proportionate to the change in flow. (Note: P1 will remain relatively constant because it is determined by aortic pressure; therefore, P2 decreases as the pressure gradient increases.) The reduction in P2 will cause P3 to decrease, reducing the perfusion pressure to the LAD vascular beds. When this occurs, FLAD will decrease. Remember that RLAD is already minimal (i.e., maximally dilated) because of the low P3 and therefore is incapable of dilating further in response to a vasodilator stimulus. The net result is that CFX blood flow increases while LAD blood flow decreases (i.e., vascular steal). This redistribution of flow leads to ischemia and hypoxia (especially during augmented oxygen demand) in the myocardium supplied by the LAD.
You can view a 26-minute YouTube lecture on this topic by clicking on Hemodynamics of Coronary Vascular Steal.
Analogous situations in the iliac and femoral circulations of the lower limb can lead to vascular steal during exercise. This is termed "intermittent claudication" and results in ischemic pain during walking.
Revised 12/27/2022

 Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021)
Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021) Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)
Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)