Hypotension - Introduction
Definition of Hypotension and its Causes
Hypotension is a physiologic state in which the arterial blood pressure is abnormally low. For an adult, hypotension exists when the systolic pressure is less than 90 mmHg and the diastolic pressure is less than 60 mmHg. Hypotension reduces blood flow and therefore oxygen delivery to organs and tissues, which may cause cellular damage and dysfunction. When oxygen delivery does not support tissue metabolic requirements, a person is said to be in circulatory shock. Because arterial pressure is determined by cardiac output, venous pressure and systemic vascular resistance (Click here for more details), a reduction in any of these variables can lead to hypotension. Hypotension may result from:
- Reduced cardiac output
- Hypovolemia (low blood volume)
- Blood volume redistribution
- Reduced systemic vascular resistance (systemic vasodilation)
- Vascular obstruction (e.g., pulmonary embolism)
The diagram shows diseases or conditions that may cause reduced cardiac output, or those related to abnormal vascular function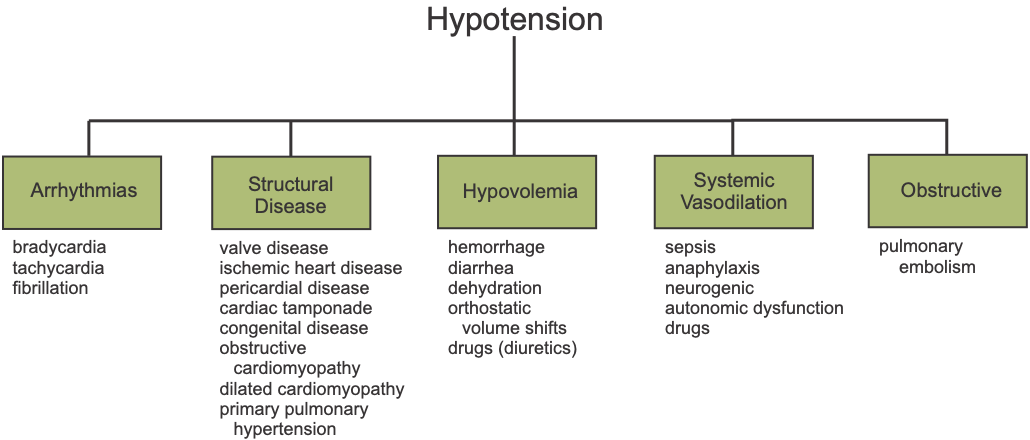 .
.
Hypotension of Cardiac Origin
Reduced cardiac output that cannot be compensated by neurohumoral reflexes can cause hypotension, which can lead to shock. If impaired cardiac output is caused by a problem with the pumping ability of the heart (e.g., arrhythmias or heart disease), then the term cardiogenic shock is used to describe the origin of the shock state.
Cardiac arrhythmias
Bradycardia caused by an abnormally slow sinus rate or resulting from an atrioventricular block that reduces ventricular rate leads to a decrease in cardiac output. Very high heart rates (tachycardia), by reducing ventricular filling time, can reduce stroke volume and, therefore, cardiac output. Ventricular fibrillation causes cardiac output to fall to zero and therefore leads to profound hypotension.
Cardiac structural disease
Cardiomyopathies (diseases of the myocardium) can impair either systolic function (inotropic state) or diastolic function (ventricular filling) and reduce cardiac output and arterial pressure. Structural diseases such as restrictive cardiomyopathy or pericarditis can impair ventricular filling and therefore reduce cardiac output. Valve disease, pericardial disease, and congenital defects can impair ventricular filling or net forward flow, reducing cardiac output. Ischemic heart disease caused by atherosclerosis or thromboembolism impairs ventricular function. Primary pulmonary hypertension can lead to right ventricular failure and impaired left ventricular filling and output.
Hypotension of Vascular Origin
Hypovolemia
Hypovolemia caused by blood loss (hemorrhage), or orthostatic volume shifts, decreases central venous pressure and ventricular filling (preload), which reduces cardiac output through the Frank-Starling mechanism. However, reduced cardiac output under these circumstances is because of inadequate cardiac filling from the systemic vasculature, not to impaired intrinsic function. Hypovolemia can also result from excessive water loss (dehydration) caused by profuse sweating, restricted water intake, or the use of diuretic drugs. Although hypovolemia reduces cardiac output, the heart itself is not the origin (non-cardiogenic), and therefore the term hypovolemic shock is used to describe the shock state that results from hypovolemic hypotension.
Systemic vasodilation
Hypotension can also be caused by excessive systemic vasodilation (decreased systemic vascular resistance). This may result from sepsis (blood infections) leading to septic shock, anaphylaxis (immunological reactions) that can lead to anaphylactic shock, autonomic dysfunction (e.g., diabetic autonomic neuropathy; spinal cord injury) leading to neurogenic shock, or drugs (e.g., antihypertensive vasodilators). These specific causes of vasodilation-induced shock are grouped together as distributive shock.
Vascular obstruction
Another vascular origin of hypotension is vascular obstruction, such as pulmonary embolism. Vascular obstruction most frequently is caused by blood clots forming in systemic veins (e.g., deep vein thrombosis in legs) that travel to the right side of the heart and embolize in pulmonary arteries. When this occurs, venous return to the left ventricle is diminished, leading to a decrease in cardiac output and arterial pressure and a state of obstructive shock.
To understand more fully the physiology and pathophysiology of hypotension, see the Blood Pressure Regulation Tutorial.
You can view an 18-minute YouTube introductory lecture on Hypotension and Shock.
Revised 11/03/2023
 Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021)
Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021) Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)
Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)