Central Venous Pressure
Venous pressure is a term that represents the average blood pressure within the venous compartment. The term "central venous pressure" (CVP) describes the pressure in the thoracic vena cava near the right atrium (therefore CVP and right atrial pressure are essentially the same). CVP is an important concept in clinical cardiology because it is a major determinant of the filling pressure and therefore the preload of the right ventricle, which regulates stroke volume through the Frank-Starling mechanism.
A change in CVP (ΔCVP) is determined by the change in volume (ΔV) of blood within the thoracic veins divided by the compliance (Cv) of the veins according to the following equation:
ΔCVP = ΔV / Cv
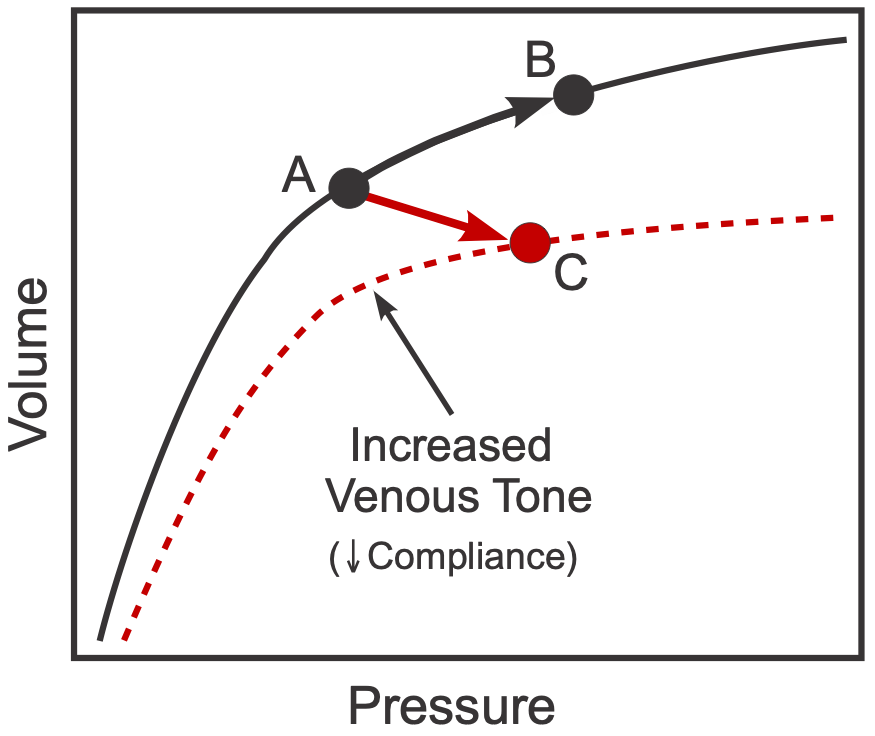 Therefore, CVP is increased by either an increase in venous blood volume or by a decrease in venous compliance. The latter change can be caused by contraction of the smooth muscle within the veins, which increases the venous vascular tone and decreases compliance. The effects of increased venous blood volume and decreased venous compliance on CVP are illustrated in the figure. Point A represents a control operating point on a compliance curve for a large vein. If the volume of blood within the vein is increased, then the operating point will shift up and to the right (from A to B) along the same compliance curve. This will lead to an increase in pressure that is determined by the change in volume and the venous compliance (slope of the curve). Venous pressure is also increased if venous smooth muscle contraction is enhanced (e.g., by sympathetic nerve stimulation). When this occurs, the venous compliance decreases (dashed red line), and the new operating point C will reflect a smaller venous volume but at a greater venous pressure.
Therefore, CVP is increased by either an increase in venous blood volume or by a decrease in venous compliance. The latter change can be caused by contraction of the smooth muscle within the veins, which increases the venous vascular tone and decreases compliance. The effects of increased venous blood volume and decreased venous compliance on CVP are illustrated in the figure. Point A represents a control operating point on a compliance curve for a large vein. If the volume of blood within the vein is increased, then the operating point will shift up and to the right (from A to B) along the same compliance curve. This will lead to an increase in pressure that is determined by the change in volume and the venous compliance (slope of the curve). Venous pressure is also increased if venous smooth muscle contraction is enhanced (e.g., by sympathetic nerve stimulation). When this occurs, the venous compliance decreases (dashed red line), and the new operating point C will reflect a smaller venous volume but at a greater venous pressure.
It is important to note for a proper conceptual understanding that the compliance of the large thoracic veins (especially the vena cava) does not undergo large changes. Instead, the major site for venous compliance changes is smaller veins located outside of the thorax. These smaller veins can undergo large changes in compliance. When the compliance of veins decreases (e.g., by sympathetic nerve stimulation) causing venoconstriction, the pressure within the veins increases and this is transmitted up to the thoracic veins, which increases their volume and pressure.
In the body, venous compliance and venous volume are not static, but dynamic, with many factors influences these two variables, such as cardiac output, respiratory activity, contraction of skeletal muscles (particularly legs and abdomen), sympathetic vasoconstrictor tone, and hydrostatic forces (i.e., gravity). Venodilator drugs, which are often used in the treatment of acute heart failure and angina, relax venous vessels (increase their compliance) and lower central venous pressure. All the above factors influence central venous pressure by either changing thoracic venous blood volume or venous compliance. These factors or mechanisms are summarized in the following table:
Factors Increasing Central Venous Pressure |
Primarily a change in compliance (C) or volume (V) |
| Decreased cardiac output | V |
| Increased blood volume | V |
| Venous constriction | C |
| Changing from standing to supine body posture | V |
| Arterial dilation | V |
| Forced expiration (e.g., Valsalva) | C |
| Muscle contraction (abdominal and limb) | V, C |
- A decrease in cardiac output either due to decreased heart rate or stroke volume (e.g., in ventricular failure) results in blood backing up into the venous circulation (increased venous volume) as less blood is pumped into the arterial circulation. The resultant increase in thoracic blood volume increases CVP.
- An increase in total blood volume as occurs in renal failure or fluid retention through activation of the renin-angiotensin-aldosterone system increases venous pressure.
- Venous constriction caused by sympathetic activation of veins, or by circulating vasoconstrictor substances (e.g., catecholamines, angiotensin II) decreases venous compliance, which increases CVP.
- A shift in blood volume into the thoracic venous compartment that occurs when a person changes from standing to supine position increases CVP.
- Arterial dilation as occurs during withdrawal of sympathetic tone or with arterial vasodilator drugs causes increased blood flow from the arterial into the venous compartments. This increases venous blood volume and CVP. This occurs when the heart is functioning normally. It is important to note, however, that arterial dilation in ventricular failure leads to a decrease in CVP instead of an increase. This occurs because the arterial dilation decreases afterload on the ventricle, leading to an increase in stroke volume. Ventricular stroke volume is more strongly influenced by afterload when the ventricular is in failure than when it has normal function.
- CVP is also increased during a force expiration, particularly against a high resistance (as occurs with a Valsalva maneuver) because of external compression of the thoracic vena cava as intrapleural pressure rises. This mechanical compression of the vena cava functionally reduces the compliance of the vena cava.
- Muscle contraction, particularly in the limbs and abdomen, compresses the veins (i.e., decreases compliance) and forces blood into the thoracic compartment, increasing thoracic blood volume and CVP.
Revised 01/30/2023

 Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021)
Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021) Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)
Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)