Cardiogenic Shock
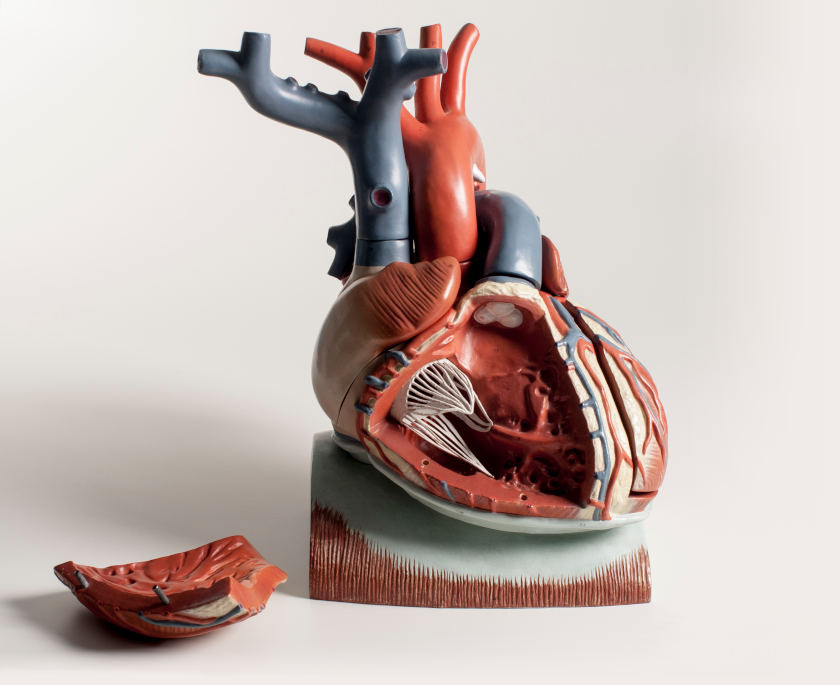
Cardiogenic shock is a clinical syndrome resulting from decreased blood flow and oxygen delivery to vital organs caused by a sustained reduction in cardiac output. This can be caused by cardiac muscle disease (e.g., cardiomyopathies), cardiac valve disease and other structural pathologies (e.g., congenital defects, ruptured chordae tendineae), sustained arrhythmias, ischemic coronary artery disease, reperfusion injury (e.g., following cardiopulmonary bypass) and myocardial infarction, which is the most common cause. Cardiogenic shock may also result from cardiac tamponade, a condition caused by an accumulation of fluid within the pericardial sac surrounding the heart. Although this is also considered being obstructive shock, this condition impairs ventricular filling and reduces cardiac output and organ perfusion. In summary, cardiogenic shock is a form of heart failure that results in significant hypotension, impaired organ perfusion, and tissue hypoxia.
Cardiogenic shock is defined as a sustained reduction in systolic pressure of <90 mmHg caused by a cardiac index of less than 2.2 liters/min/mm2. The cardiac index is the cardiac output divided by the estimated surface area of the body. This calculation normalizes cardiac output values to different size individuals and normally ranges from 2.6 to 4.2 liters/min/m2. Reduced cardiac output is usually accompanied by a compensatory, baroreceptor-mediated increase in heart rate. As in other forms of heart failure, ventricular filling pressures increase. This is caused by blood backing up into the venous circulation and by a compensatory increase in blood volume stimulated by the renin-angiotensin-aldosterone system (RAAS). The increase in venous pressures can lead to pulmonary and systemic edema.
Baroreceptor reflexes not only increase heart rate, but they also increase systemic vascular resistance, particularly in skeletal muscle, gastrointestinal, renal and cutaneous circulations. Vasoconstriction in these organs partially offsets the fall in arterial pressure, and therefore helps to maintain perfusion of the brain and heart circulations; however, blood flow can be profoundly reduced in the constricted organs, which can speed up their damage. Hypotension and renal pre-glomerular vasoconstriction decreases glomerular filtration, and increases sodium and water retention. Activation of RAAS further increases sodium and water retention to increase blood volume. The angiotensin II also produces systemic vasoconstriction directly through vascular AT1 receptors and indirectly by enhancing sympathetic activity to the vasculature.
Like hemorrhagic shock, prolonged hypotension and impaired organ perfusion can activate decompensatory mechanisms that lead to irreversible shock and death.
Revised 11/04/2023
 Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021)
Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021) Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)
Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)