Viscosity of Blood
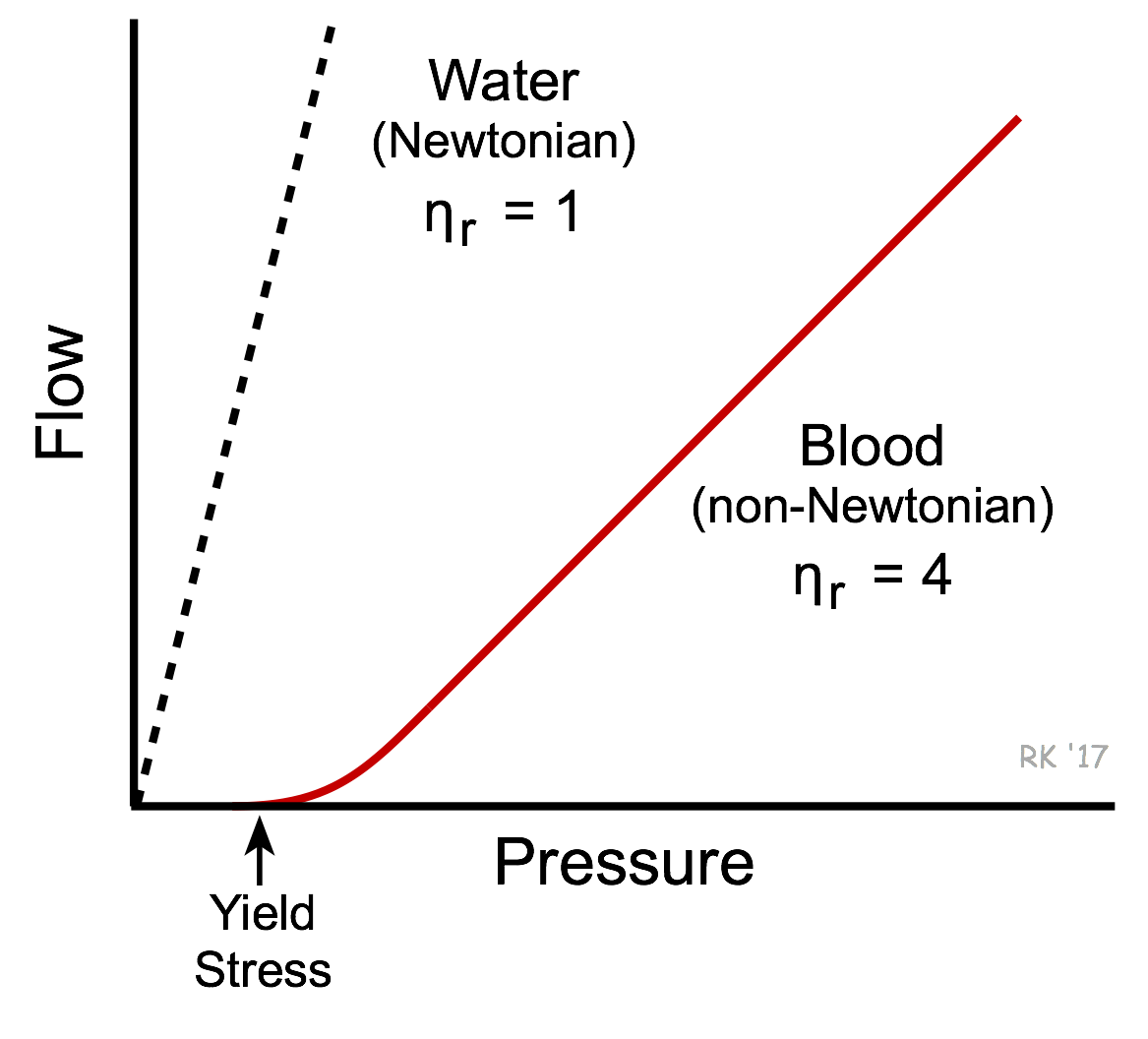 Viscosity is an intrinsic property of fluid related to the internal friction of adjacent fluid layers sliding past one another (see laminar flow). This internal friction contributes to the resistance to flow, as described by Poiseuille's equation. The interactions between fluid layers depend on the chemical nature of the fluid, and whether it is homogeneous or heterogeneous in composition. For example, water is a homogeneous fluid and its viscosity is determined by molecular interactions between water molecules. Water behaves as a Newtonian fluid and therefore, under non-turbulent conditions, its viscosity is independent of flow velocity (i.e., viscosity does not change with changes in velocity). This is shown in the figure as a linear dashed line for the flow-pressure relationship of water. There is an inverse relationship between flow and viscosity; therefore, the greater the viscosity, the smaller the slope of the flow-pressure relationship. Therefore, flow is reduced at a given driving pressure when viscosity is elevated. Whole blood has a much higher viscosity than water and therefore the slope of the flow-pressure relationship is less steep (see figure). Unlike water, blood is non-Newtonian because its viscosity increases at low flow velocities (e.g., during circulatory shock). Low flow states permit increased molecular interactions to occur between red cells and between plasma proteins and red cells. This can cause red cells to stick together and form chains of several cells (rouleaux formation) within the microcirculation, which increases the blood viscosity. Because of the high interaction between the elements of blood when it is not flowing, a driving pressure significantly greater than zero is required for stationary blood to flow again. This is referred to as the yield stress required to start flow.
Viscosity is an intrinsic property of fluid related to the internal friction of adjacent fluid layers sliding past one another (see laminar flow). This internal friction contributes to the resistance to flow, as described by Poiseuille's equation. The interactions between fluid layers depend on the chemical nature of the fluid, and whether it is homogeneous or heterogeneous in composition. For example, water is a homogeneous fluid and its viscosity is determined by molecular interactions between water molecules. Water behaves as a Newtonian fluid and therefore, under non-turbulent conditions, its viscosity is independent of flow velocity (i.e., viscosity does not change with changes in velocity). This is shown in the figure as a linear dashed line for the flow-pressure relationship of water. There is an inverse relationship between flow and viscosity; therefore, the greater the viscosity, the smaller the slope of the flow-pressure relationship. Therefore, flow is reduced at a given driving pressure when viscosity is elevated. Whole blood has a much higher viscosity than water and therefore the slope of the flow-pressure relationship is less steep (see figure). Unlike water, blood is non-Newtonian because its viscosity increases at low flow velocities (e.g., during circulatory shock). Low flow states permit increased molecular interactions to occur between red cells and between plasma proteins and red cells. This can cause red cells to stick together and form chains of several cells (rouleaux formation) within the microcirculation, which increases the blood viscosity. Because of the high interaction between the elements of blood when it is not flowing, a driving pressure significantly greater than zero is required for stationary blood to flow again. This is referred to as the yield stress required to start flow.
Although plasma is mostly water, it also contains molecules such as electrolytes and proteins (especially albumin and fibrinogen). Because of molecular interactions between these different components of plasma, it is not surprising that plasma has a higher viscosity than water. In fact, plasma at 37°C is about 1.8-times more viscous than water at the same temperature; therefore, the relative viscosity (ηr) of plasma compared to water is about 1.8.
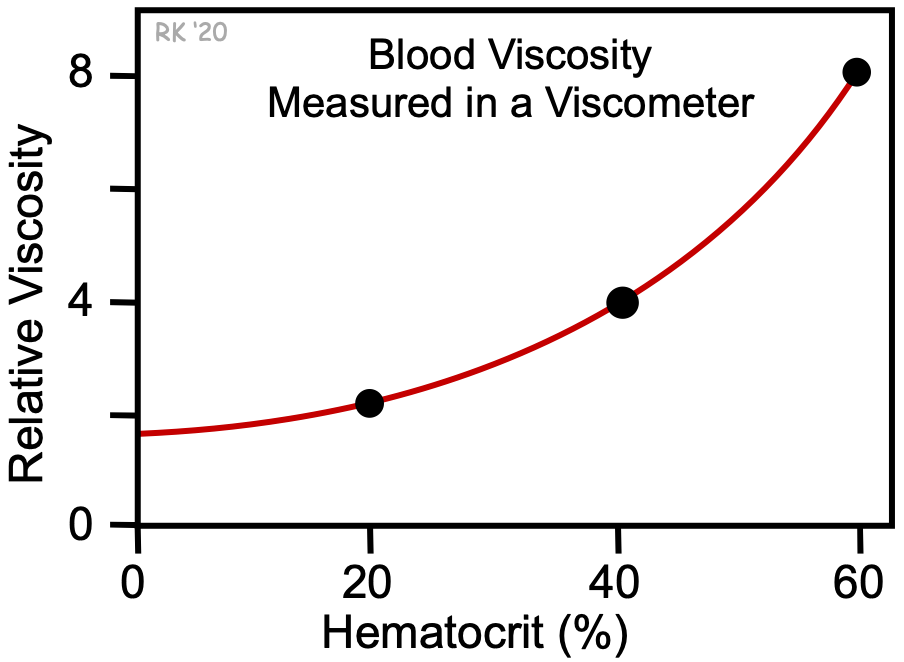 The addition of formed elements to plasma (red cells, white cells, and platelets) further increases the viscosity. Of these formed elements, red cells have the greatest effect on viscosity. In the figure, the relative viscosity at 0% hematocrit (plasma without cells) is about 1.8, as shown by the y-intercept. Increasing red cell hematocrit increases relative viscosity. Note that the increase is non-linear; increased hematocrit causes a disproportionate increase in relative viscosity. Therefore, blood viscosity strongly depends on hematocrit. At a normal hematocrit of 40%, the relative viscosity of blood is about 4. Patients with an abnormal elevation in red cell hematocrit (polycythemia) have much higher blood viscosities. In fact, increasing the hematocrit from 40 to 60% (a 50% increase) increases the relative viscosity from 4 to 8 (a 100% increase). Increased viscosity increases the resistance to blood flow and increases the work of the heart and impairs organ perfusion. Some patients with anemia have low hematocrits, and therefore reduced blood viscosities.
The addition of formed elements to plasma (red cells, white cells, and platelets) further increases the viscosity. Of these formed elements, red cells have the greatest effect on viscosity. In the figure, the relative viscosity at 0% hematocrit (plasma without cells) is about 1.8, as shown by the y-intercept. Increasing red cell hematocrit increases relative viscosity. Note that the increase is non-linear; increased hematocrit causes a disproportionate increase in relative viscosity. Therefore, blood viscosity strongly depends on hematocrit. At a normal hematocrit of 40%, the relative viscosity of blood is about 4. Patients with an abnormal elevation in red cell hematocrit (polycythemia) have much higher blood viscosities. In fact, increasing the hematocrit from 40 to 60% (a 50% increase) increases the relative viscosity from 4 to 8 (a 100% increase). Increased viscosity increases the resistance to blood flow and increases the work of the heart and impairs organ perfusion. Some patients with anemia have low hematocrits, and therefore reduced blood viscosities.
Another important factor that influences blood viscosity is temperature. Just like molasses, when blood gets cold, it becomes "thicker" and flows more slowly. Therefore, there is an inverse relationship between temperature and viscosity. Viscosity increases about 2% for each degree centigrade decrease in temperature. Normally, blood temperature does not change much in the body. However, if a person's hand is exposed to a cold environment and the fingers become cold, the blood temperature in the fingers falls and viscosity increases, which, together with sympathetic-mediated vasoconstriction, decreases blood flow in the cooled region. When whole body hypothermia is induced in critical care or surgical situations, this leads to an increase in blood viscosity and impaired organ blood flow.
If clotting mechanisms are stimulated in the blood, platelet aggregation and interactions with plasma proteins occur. This leads to entrapment of red cells and clot formation, which dramatically increases blood viscosity.
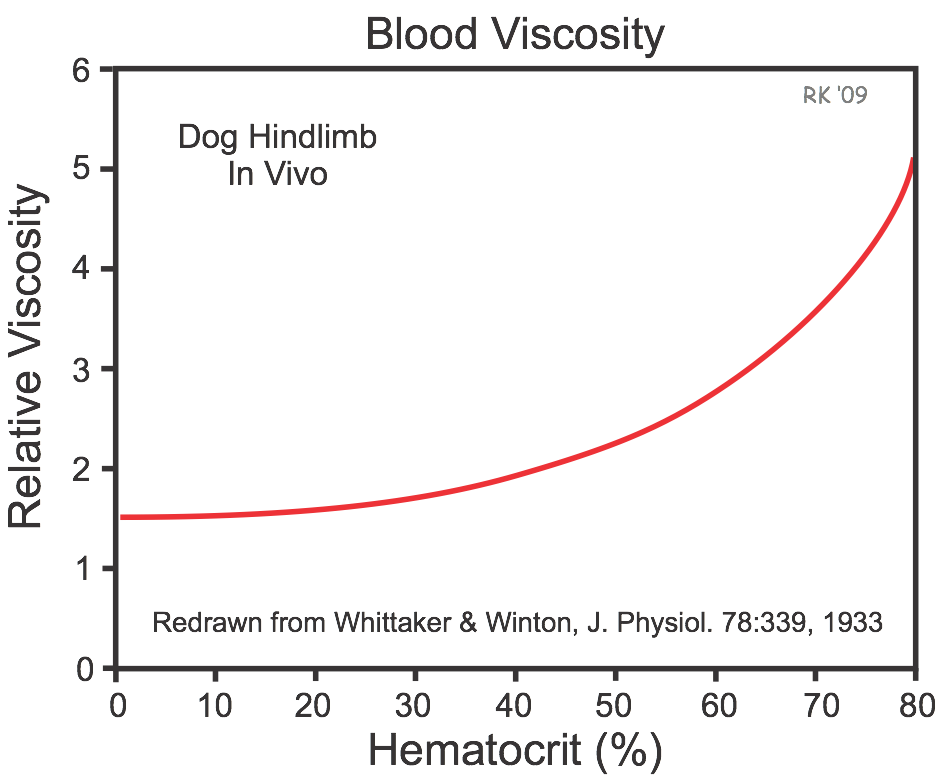 There is a microcirculatory phenomenon called the Fahraeus-Lindqvist effect that leads to a reduction in hematocrit in small arterioles (less than 200 microns in diameter) and capillaries relative to the hematocrit of large feed arteries. This decrease in hematocrit in these flowing vessels reduces the relative blood viscosity in the small vessels, which helps to offset the increase in viscosity that can occur because of reduced velocity in these same vessels. The net effect of these changes is that blood flow in the microcirculation has a lower viscosity than what is predicted by in vitro blood viscometer measurements. To illustrate this phenomenon, in vivo measurements of blood viscosity made in dog hindlimbs by Whittaker and Winton (J. Physiol. 78:339, 1933) showed that at a measured arterial blood hematocrit, the relative viscosity of blood flowing in the hindlimb is much lower than predicted from in vitro experiments (compare figure at right with previous figure that used a viscometer).
There is a microcirculatory phenomenon called the Fahraeus-Lindqvist effect that leads to a reduction in hematocrit in small arterioles (less than 200 microns in diameter) and capillaries relative to the hematocrit of large feed arteries. This decrease in hematocrit in these flowing vessels reduces the relative blood viscosity in the small vessels, which helps to offset the increase in viscosity that can occur because of reduced velocity in these same vessels. The net effect of these changes is that blood flow in the microcirculation has a lower viscosity than what is predicted by in vitro blood viscometer measurements. To illustrate this phenomenon, in vivo measurements of blood viscosity made in dog hindlimbs by Whittaker and Winton (J. Physiol. 78:339, 1933) showed that at a measured arterial blood hematocrit, the relative viscosity of blood flowing in the hindlimb is much lower than predicted from in vitro experiments (compare figure at right with previous figure that used a viscometer).
Revised 12/27/2022

 Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021)
Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021) Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)
Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)