Hemodynamics of Single and Multiple Arterial Stenotic Lesions
Single Arterial Stenosis
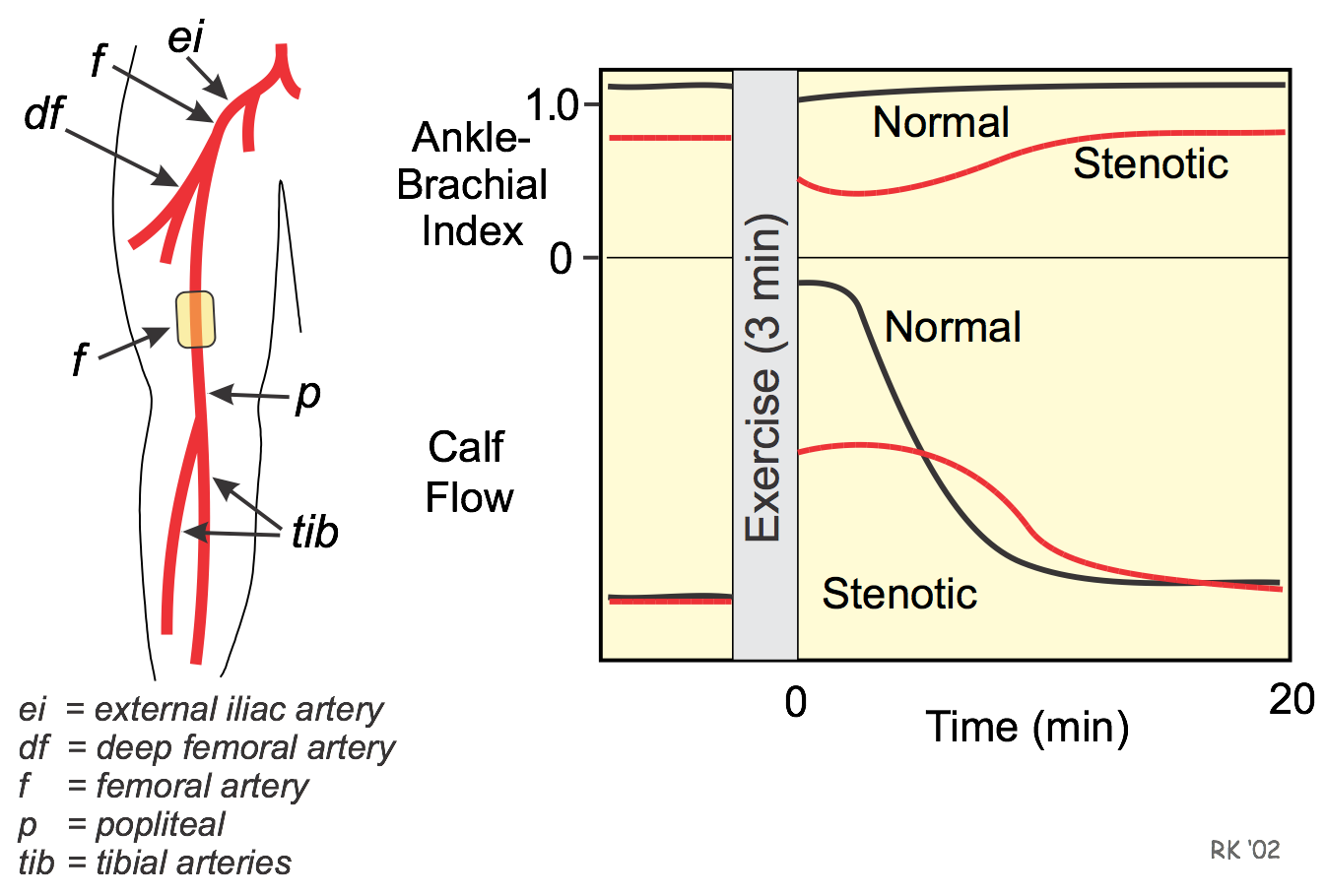 A single arterial stenotic lesion in the femoral artery distal to the deep femoral branch, for example (see figure), can decrease resting blood flow and maximal flow capacity to the tissues supplied by the femoral artery (e.g., calf musculature). A lesion at this site reduces pressure distal to the lesion because the increased resistance increases the pressure drop along the length of the stenotic segment. If the pressure drop is relatively small at resting flows (e.g., 10-30 mmHg), autoregulation and collateralization can reduce the resistance in the distal vascular beds sufficiently to maintain resting blood flow. For this reason, measuring blood flow (e.g., by Doppler techniques) under resting conditions in a limb will not always detect stenotic lesions because flow may be normal. However, measuring pressures at different sites in the limb (i.e., measuring segmental pressures) or determining the ankle-brachial pressure index will detect stenotic lesions.
A single arterial stenotic lesion in the femoral artery distal to the deep femoral branch, for example (see figure), can decrease resting blood flow and maximal flow capacity to the tissues supplied by the femoral artery (e.g., calf musculature). A lesion at this site reduces pressure distal to the lesion because the increased resistance increases the pressure drop along the length of the stenotic segment. If the pressure drop is relatively small at resting flows (e.g., 10-30 mmHg), autoregulation and collateralization can reduce the resistance in the distal vascular beds sufficiently to maintain resting blood flow. For this reason, measuring blood flow (e.g., by Doppler techniques) under resting conditions in a limb will not always detect stenotic lesions because flow may be normal. However, measuring pressures at different sites in the limb (i.e., measuring segmental pressures) or determining the ankle-brachial pressure index will detect stenotic lesions.
Because resting blood flow with mild-to-moderate stenosis is not necessarily compromised, ischemic pain may not be present at rest. With more severe stenosis of the femoral artery, the pressure drop is greater and the autoregulatory capacity of the distal vascular beds may be exceeded, leading to a fall in resting blood flow. When this occurs, the patient will experience ischemic pain (and other pathologies associated with ischemia) at rest.
During limb exercise (see previous figure), a patient with a stenotic lesion in the femoral artery distal to the deep femoral branch may experience ischemic pain in the calf musculature supplied by the femoral artery. This occurs because the maximal blood flow capacity to the calf is limited by the increased resistance in the femoral artery. This distribution artery is in-series with the calf vasculature; therefore, the resistances are additive and total resistance to blood flow is higher than in the absence of the proximal stenosis when the circulation in the calf musculature is maximally dilated. With normal vessels, the ankle-brachial pressure index does not fall appreciably during the phase of active hyperemia because the resistance is very low in the distributing arteries. When resistance is increased by stenosis, the resting ankle-brachial pressure index is reduced, and the index falls even further when the distal beds dilate during exercise. This distal dilation increases flow across the stenotic segment, further increasing the pressure drop across the lesion. This reduced pressure effectively reduces the perfusion pressure to the distal vascular beds, which decreases maximal blood flow to the calf during exercise.
It should be noted that a lesion in the femoral artery distal to the deep femoral branch will not alter blood flow to proximal vascular beds (e.g., those supplied by the deep femoral or internal iliac arteries). Flow in those proximal tissues only depends on their arterial perfusion pressure and vascular resistance, neither of which will be changed by a distal lesion.
Multiple Arterial Stenoses
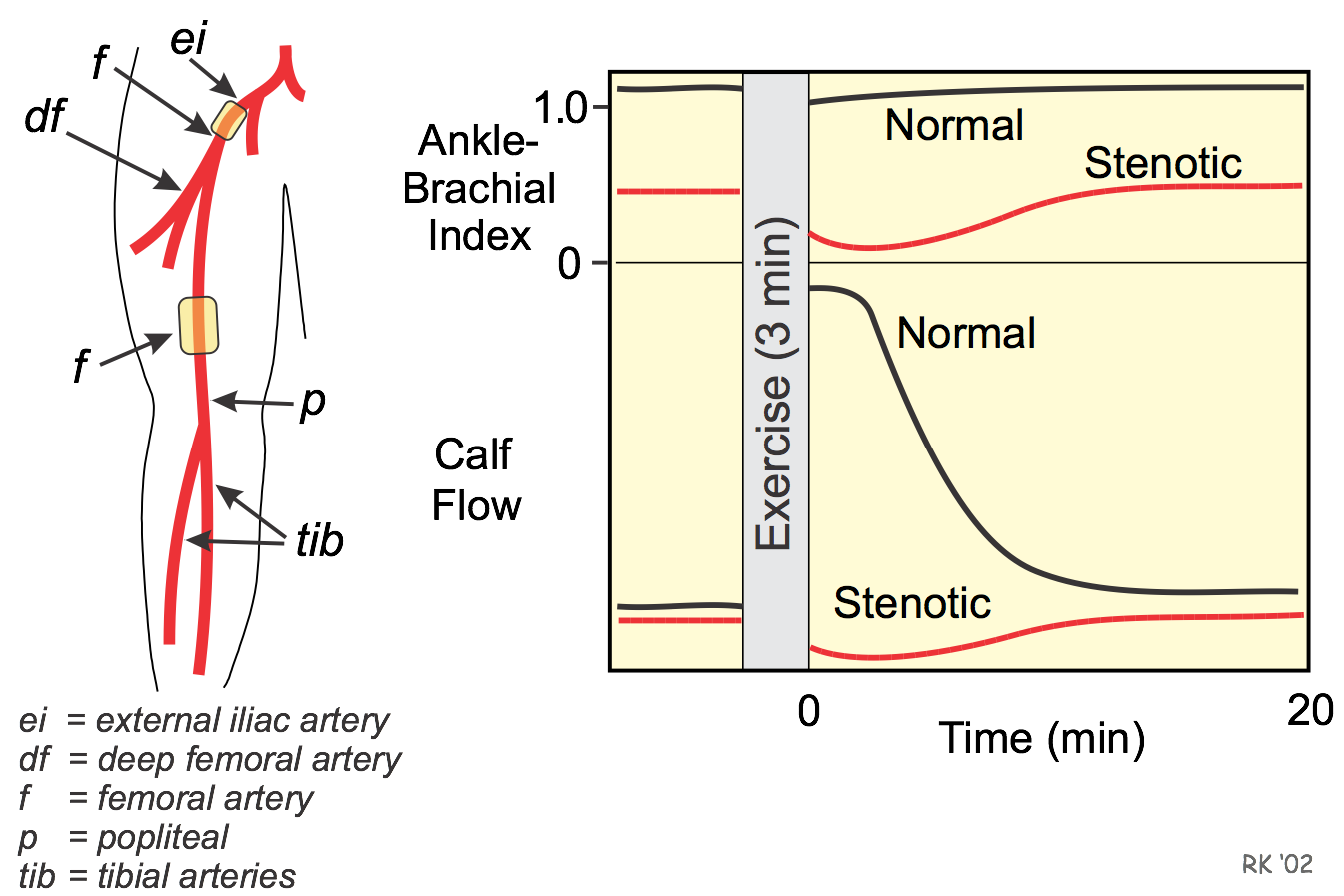 The hemodynamics associated with a single stenotic lesion are significantly compounded by a second lesion. Consider, for example, stenotic lesions in both the femoral artery distal to the deep femoral and in the external iliac artery as shown in the figure. Under resting, non-exercise conditions, blood flow may or may not be reduced in the deep femoral and tibial circulations, depending on the extent of autoregulation and collateralization. The calf circulation will more likely be compromised at rest because there are two proximal (and in-series) stenotic lesions. In contrast, the deep femoral circulation to the thigh is distal to only one stenotic lesion and is therefore less likely to be compromised at rest. Regardless of the resting blood flows, the pressures distal to the lesions will be reduced. Because there are two in-series stenoses proximal to the ankle, the ankle-brachial pressure index may be considerably reduced, even under resting conditions. If it is assumed that the perfusion pressure to the calf is reduced to where the microvasculature is maximally dilated (i.e., maximal autoregulation has occurred), then exercising the limb will cause blood flow to decrease in the calf (termed vascular steal) as shown in the figure. This happens because as the vessels dilate in the thigh during exercise (assuming they have not already dilated to their maximal autoregulatory capacity), the pressure distal to the external iliac lesion will fall (the increased flow increases the pressure drop across the lesion) further reducing the perfusion pressure to the lower leg and causing calf blood flow to fall. The hemodynamic principles governing vascular steal in the leg are the same principles that describe coronary vascular steal. After exercise, the microcirculation in the thigh regains its vascular tone, causing the perfusion pressure to the calf to rise and calf blood flow to increase. The fall in calf blood flow during limb exercise occurs at the time the calf musculature is contracting and for several minutes thereafter. This leads to a significant reduction in the oxygen supply/demand ratio during limb contraction, which can lead to ischemic pain (i.e., intermittent claudication) in the calf.
The hemodynamics associated with a single stenotic lesion are significantly compounded by a second lesion. Consider, for example, stenotic lesions in both the femoral artery distal to the deep femoral and in the external iliac artery as shown in the figure. Under resting, non-exercise conditions, blood flow may or may not be reduced in the deep femoral and tibial circulations, depending on the extent of autoregulation and collateralization. The calf circulation will more likely be compromised at rest because there are two proximal (and in-series) stenotic lesions. In contrast, the deep femoral circulation to the thigh is distal to only one stenotic lesion and is therefore less likely to be compromised at rest. Regardless of the resting blood flows, the pressures distal to the lesions will be reduced. Because there are two in-series stenoses proximal to the ankle, the ankle-brachial pressure index may be considerably reduced, even under resting conditions. If it is assumed that the perfusion pressure to the calf is reduced to where the microvasculature is maximally dilated (i.e., maximal autoregulation has occurred), then exercising the limb will cause blood flow to decrease in the calf (termed vascular steal) as shown in the figure. This happens because as the vessels dilate in the thigh during exercise (assuming they have not already dilated to their maximal autoregulatory capacity), the pressure distal to the external iliac lesion will fall (the increased flow increases the pressure drop across the lesion) further reducing the perfusion pressure to the lower leg and causing calf blood flow to fall. The hemodynamic principles governing vascular steal in the leg are the same principles that describe coronary vascular steal. After exercise, the microcirculation in the thigh regains its vascular tone, causing the perfusion pressure to the calf to rise and calf blood flow to increase. The fall in calf blood flow during limb exercise occurs at the time the calf musculature is contracting and for several minutes thereafter. This leads to a significant reduction in the oxygen supply/demand ratio during limb contraction, which can lead to ischemic pain (i.e., intermittent claudication) in the calf.
Revised 01/24/2024

 Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021)
Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021) Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)
Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)