Skeletal Muscle Blood Flow
The regulation of skeletal muscle blood flow is important because skeletal muscle serves important locomotory functions in the body. Contracting muscle consumes large amounts of oxygen to replenish ATP that is hydrolyzed during contraction; therefore, contracting muscle needs to increase its blood flow and oxygen delivery to support its metabolic and contractile activities. As in all tissues, the microcirculation, particularly small arteries and arterioles, is the most influential site for regulating vascular resistance and blood flow within the muscle. Like cardiac muscle, each muscle fiber (cell) is surrounded by several capillaries. This reduces diffusion distances for the efficient exchange of gases (O2 and CO2) and other molecules between the blood and the skeletal muscle cells.
Characteristics of Skeletal Muscle Blood Flow
- Skeletal muscle accounts for about 20% of cardiac output at rest. During strenuous physical exertion, over 80% of cardiac output can be directed to contracting muscles, which undergo extensive vasodilation to enable the increase in flow. When this occurs, systemic vascular resistance decreases, which attenuates the increase in arterial pressure that would otherwise occur with a large increase in cardiac output during strenuous exercise.
- At rest, skeletal muscle blood flows may be 1-4 mL/min per 100g; maximal blood flows may reach 50-100 mL/min per 100g, depending on the muscle type. Therefore, blood flow can increase 20 to 50-fold with maximal vasodilation or active hyperemia.
- Coordinated, rhythmical contractions (e.g., running) enhance blood flow by the skeletal muscle pump mechanism.
- Sympathetic innervation produces vasoconstriction through alpha1 and alpha2 adrenoceptors on the vascular smooth muscle. There is a significant amount of sympathetic tone at rest so that abrupt removal of sympathetic influences (e.g., by using an alpha-adrenoceptor blocker) can increase resting flow 2 to 3-fold.
- Vascular beta2-adrenoceptors produce vasodilation when stimulated by agonists such as epinephrine.
- There is evidence for sympathetic cholinergic innervation of skeletal muscle arteries in some species, such as dogs and cats; however, there is no convincing evidence that this occurs in human skeletal muscle. In species having sympathetic cholinergic innervation, activation during exercise can cause vasodilation through the release of acetylcholine binding to muscarinic receptors.
- There is a tight coupling between oxygen consumption and blood flow.
- Blood flow is determined by local regulatory (tissue and endothelial) factors, such as tissue hypoxia, adenosine, K+, CO2, H+, and nitric oxide. During exercise, these local regulatory mechanisms override the sympathetic vasoconstrictor influences (termed functional sympatholysis).
- Skeletal muscle blood flow shows a moderate degree of autoregulation.
- Like the coronary circulation, muscle blood flow can be significantly compromised by extravascular compression that occurs during strong muscular contractions, especially during sustained tetanic contractions.
The figure below shows how blood flow changes during phasic contractions. This is observed when measuring brachial artery inflow during rhythmical contraction of the forearm.
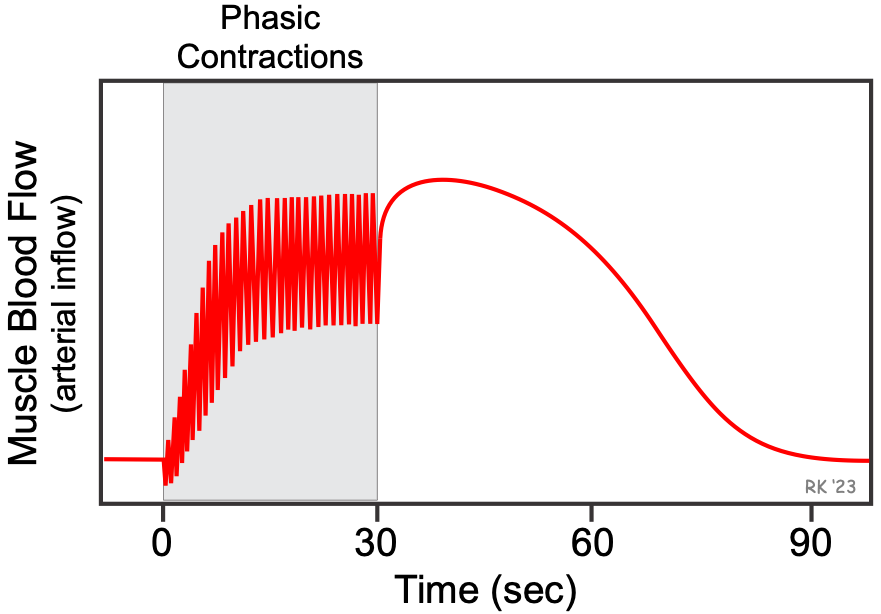 When the contractions first begin, blood flow briefly decreases because of compressive forces exerted by the contracting muscles on the vasculature within the muscle. Each time the muscles contract, arterial inflow decreases because of extravascular compression, and then arterial inflow increases as the muscles relax. This is repeated each time the muscles contract and relax. If flow were measured in the outflow vein, the venous outflow would increase during contraction and decrease during relaxation – the opposite of what occurs on the arterial side of the circulation. After just a couple of seconds, mean and peak flows increase (active hyperemia). After 15–20 seconds, the increased flow will reach a steady state that is determined by the force and frequency of contraction and the metabolic demands of the tissue. When contractions cease, blood flow may transiently increase because of the loss of compressive forces, and then, over the next few minutes, the flow returns to control.
When the contractions first begin, blood flow briefly decreases because of compressive forces exerted by the contracting muscles on the vasculature within the muscle. Each time the muscles contract, arterial inflow decreases because of extravascular compression, and then arterial inflow increases as the muscles relax. This is repeated each time the muscles contract and relax. If flow were measured in the outflow vein, the venous outflow would increase during contraction and decrease during relaxation – the opposite of what occurs on the arterial side of the circulation. After just a couple of seconds, mean and peak flows increase (active hyperemia). After 15–20 seconds, the increased flow will reach a steady state that is determined by the force and frequency of contraction and the metabolic demands of the tissue. When contractions cease, blood flow may transiently increase because of the loss of compressive forces, and then, over the next few minutes, the flow returns to control.
Revised 11/03/2023
 Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021)
Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021) Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)
Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)