Physical Factors that Determine Capillary Fluid Exchange
There is a free exchange of water, electrolytes, and small molecules between the intravascular and extravascular compartments of the body. The primary site of this exchange is capillaries and small post-capillary venules (collectively called "exchange vessels"). Several mechanisms are involved in this exchange, but the most important are bulk flow and diffusion. The rate of exchange for exchange of water and electrolytes, in either direction, is determined by physical factors: hydrostatic pressure, oncotic pressure, and the physical nature of the barrier separating the blood and interstitial compartment of the tissue (i.e., the permeability of the vessel wall).
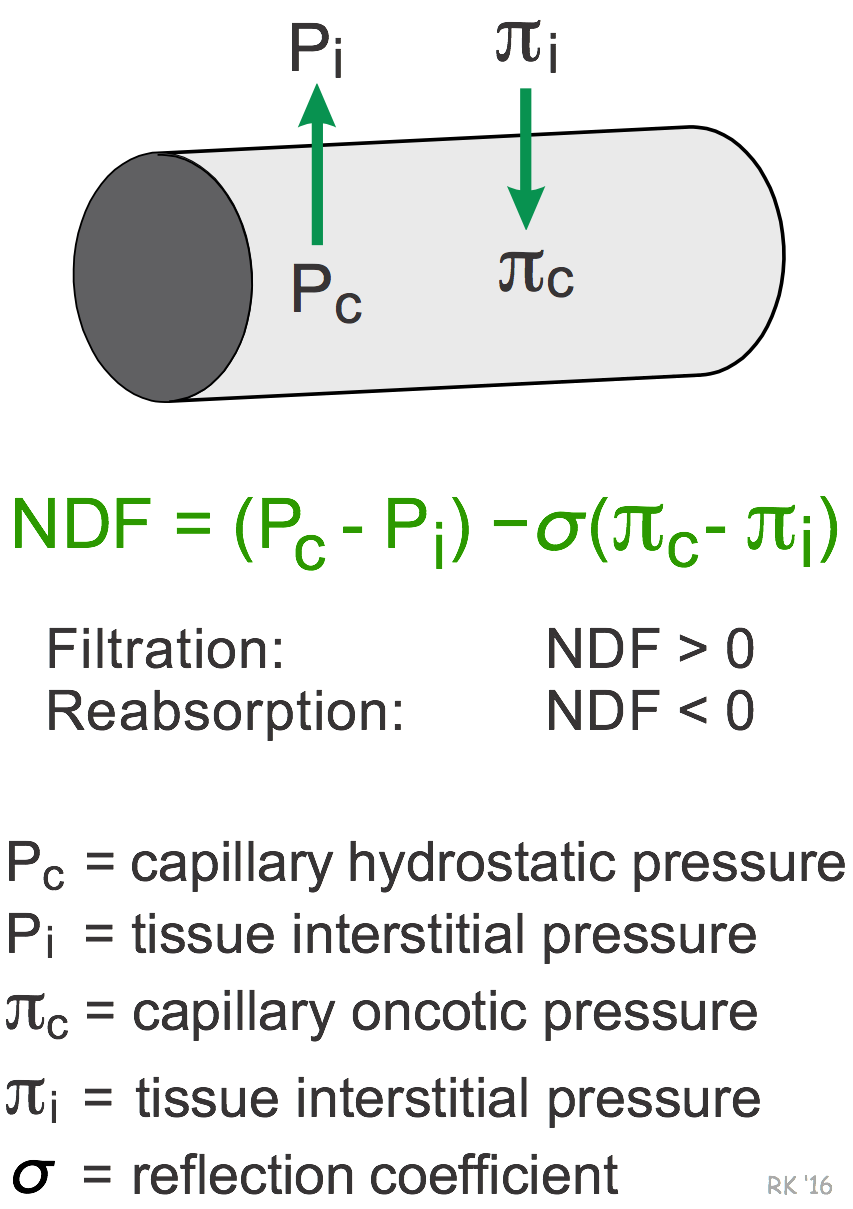 There are two significant and opposing hydrostatic forces: capillary hydrostatic pressure (Pc) and tissue interstitial pressure (Pi). Because Pc is normally much greater than Pi, the net hydrostatic pressure gradient (Pc – Pi) across the capillary is positive, meaning that hydrostatic forces are driving fluid out of the capillary and into the interstitium. There are also two opposing oncotic pressures influencing fluid exchange: capillary plasma oncotic pressure (πc) and tissue (interstitial) oncotic pressure (πi). πc is much greater than πi, therefore the net oncotic pressure gradient (πc - πi) across the capillary, if unopposed by hydrostatic forces, would reabsorb fluid from the interstitium into the capillary. The net oncotic pressure (πc - πi) should be multiplied by the reflection coefficient, which is a measure of the permeability of the capillary barrier to the proteins responsible for generating the oncotic pressure. If the capillary barrier is impermeable to protein, then the reflection coefficient is 1. The net driving force (NDF) for fluid movement is the net pressure gradient determined by the sum of the individual hydrostatic and oncotic pressures, and is expressed in the units of mmHg. When the NDF is positive, there is net fluid filtration, and when it is negative, there is net fluid reabsorption.
There are two significant and opposing hydrostatic forces: capillary hydrostatic pressure (Pc) and tissue interstitial pressure (Pi). Because Pc is normally much greater than Pi, the net hydrostatic pressure gradient (Pc – Pi) across the capillary is positive, meaning that hydrostatic forces are driving fluid out of the capillary and into the interstitium. There are also two opposing oncotic pressures influencing fluid exchange: capillary plasma oncotic pressure (πc) and tissue (interstitial) oncotic pressure (πi). πc is much greater than πi, therefore the net oncotic pressure gradient (πc - πi) across the capillary, if unopposed by hydrostatic forces, would reabsorb fluid from the interstitium into the capillary. The net oncotic pressure (πc - πi) should be multiplied by the reflection coefficient, which is a measure of the permeability of the capillary barrier to the proteins responsible for generating the oncotic pressure. If the capillary barrier is impermeable to protein, then the reflection coefficient is 1. The net driving force (NDF) for fluid movement is the net pressure gradient determined by the sum of the individual hydrostatic and oncotic pressures, and is expressed in the units of mmHg. When the NDF is positive, there is net fluid filtration, and when it is negative, there is net fluid reabsorption.
For a given NDF, the amount of fluid filtered or reabsorbed per unit time (fluid flux, or JV) is determined by the permeability of the capillary barrier and by the surface area available for exchange. The permeability is usually referred to as the filtration constant (KF), and is determined by the physical properties of the barrier (i.e., size and number of "pores" and the thickness of the barrier). For example, fenestrated capillaries have a higher KF than continuous capillaries. Substances such as histamine, which are released in response to tissue injury or inflammation, increase KF. The surface area (A) is related to the length, diameter, and number of capillaries available for exchange. The surface area is dynamic in vascular beds such as skeletal muscle, where the number of perfused capillaries increases several-fold during exercise.
To summarize: JV = KF A [(PC − Pi) − σ(πC - πi)]
The expression in brackets represents the NDF. If this is positive, filtration occurs, and if negative, reabsorption occurs. At a given NDF, the JV is determined by the product of KF and A.
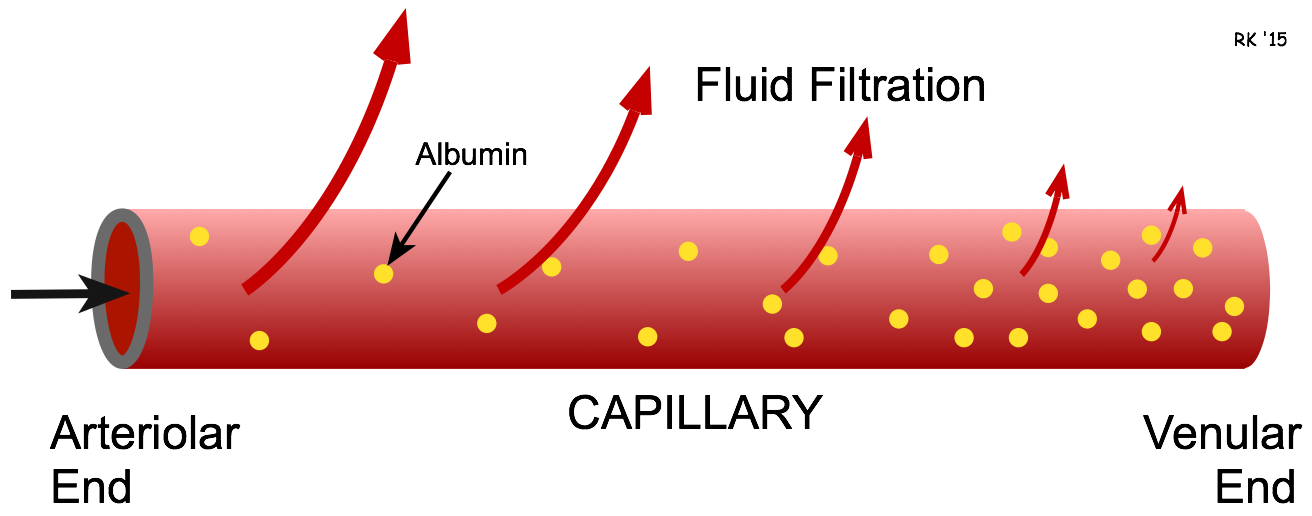 In all vascular beds of the body, filtration is greatest at the arteriolar end of the capillary because Pc is greatest at this point along a capillary. As the blood moves along the length of the capillary, the rate of fluid filtration declines. In some capillaries, fluid reabsorption occurs at the venular end of the capillary and at the small postcapillary venules. This is because the NDF has a relatively high positive value at the arteriolar end of the capillary. As the blood flows through the capillary, the capillary resistance to flow causes Pc to fall along the length of the capillary. Because fluid is filtering out of the capillary, the plasma protein (primarily albumin) concentration increases along the length of the capillary, which increases πc and further decreases the NDF. If the NDF becomes negative towards the venous end of the capillary because of decreased Pc and increased πc, then reabsorption occurs.
In all vascular beds of the body, filtration is greatest at the arteriolar end of the capillary because Pc is greatest at this point along a capillary. As the blood moves along the length of the capillary, the rate of fluid filtration declines. In some capillaries, fluid reabsorption occurs at the venular end of the capillary and at the small postcapillary venules. This is because the NDF has a relatively high positive value at the arteriolar end of the capillary. As the blood flows through the capillary, the capillary resistance to flow causes Pc to fall along the length of the capillary. Because fluid is filtering out of the capillary, the plasma protein (primarily albumin) concentration increases along the length of the capillary, which increases πc and further decreases the NDF. If the NDF becomes negative towards the venous end of the capillary because of decreased Pc and increased πc, then reabsorption occurs.
In most capillaries, there is net filtration (i.e., filtration > reabsorption) that is picked up by the lymphatics. If an imbalance occurs in which net filtration exceeds the capacity of the lymphatics, then edema results. The kidneys are an exception to these generalizations in that renal glomerular capillaries filter large amounts of fluid along their entire length. This results from higher glomerular capillary hydrostatic pressures and higher capillary permeability.
Revised 11/05/2023

 Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021)
Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021) Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)
Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)