Pulmonary Capillary Wedge Pressure
What does it measure?
Pulmonary capillary wedge pressure (PCWP) provides an indirect estimate of left atrial pressure (LAP). Although left ventricular pressure can be directly measured by placing a catheter within the left ventricle, it is not feasible to advance this catheter back into the left atrium. LAP can be measured by placing a special catheter into the right atrium, then punching through the interatrial septum; however, for obvious reasons, this is not usually performed because of damage to the septum and potential harm to the patient.
How is it measured?
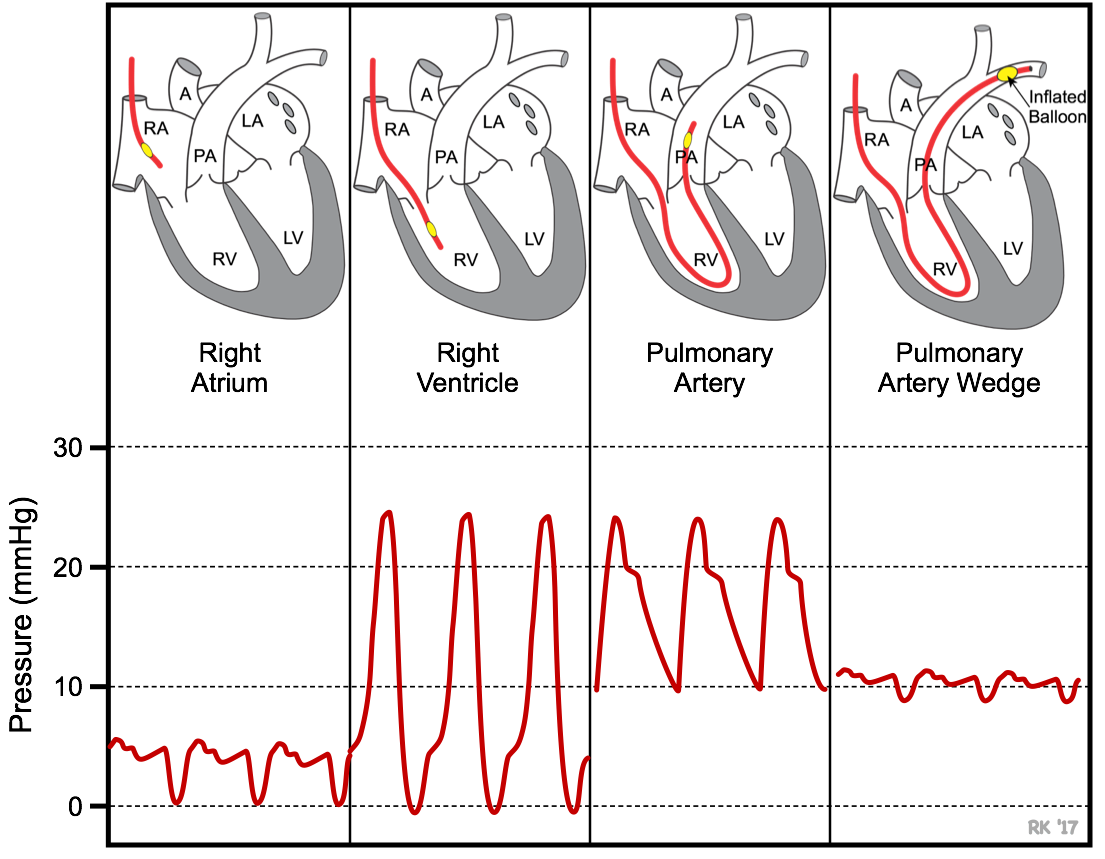 PCWP is measured by inserting a balloon-tipped, multi-lumen catheter (Swan-Ganz catheter) into a peripheral vein (e.g., jugular or femoral vein). The catheter is then advanced into the right atrium, right ventricle, pulmonary artery, and then into a branch of the pulmonary artery. The catheter has a lumen (port) that opens at the tip of the catheter distal to the balloon. This port is connected to a pressure transducer. As illustrated below, the location of the catheter can be determined by viewing the pressure measured from the tip of the catheter. In the right atrium (RA), the pressure typically averages <5 mmHg and fluctuates a few mmHg. When the catheter is advanced into the right ventricle (RV), the systolic pressure increases to ~25 mmHg and the diastolic pressure remains similar to right atrial diastolic pressure. When the catheter enters the pulmonary artery (PA), the systolic pressure normally is similar to the right ventricular systolic pressure, but the diastolic pressure increases to about 10 mmHg because of pulmonic valve closure at the beginning of diastole. Just behind the tip of the catheter is a small balloon that can be inflated with air (~1 cc). When properly positioned in a branch of the pulmonary artery, the distal port measures pulmonary artery pressure (~ 25/10 mmHg; systolic/diastolic pressure). The balloon is then inflated, which occludes the branch of the pulmonary artery. When this occurs, the pressure in the distal port rapidly falls, and after several seconds, reaches a stable lower value that is very similar to left atrial pressure (mean pressure normally 8-10 mmHg). The pressure recorded during balloon inflation approximates left atrial pressure because the occluded vessel and its distal branches that eventually form the pulmonary veins act as an extension of the catheter. The pressure fluctuates during the cardiac cycle and normally shows a, c and v waves similar to the right atrial pressure tracing. The balloon is then deflated. This same catheter can be used to measure cardiac output by the thermodilution technique.
PCWP is measured by inserting a balloon-tipped, multi-lumen catheter (Swan-Ganz catheter) into a peripheral vein (e.g., jugular or femoral vein). The catheter is then advanced into the right atrium, right ventricle, pulmonary artery, and then into a branch of the pulmonary artery. The catheter has a lumen (port) that opens at the tip of the catheter distal to the balloon. This port is connected to a pressure transducer. As illustrated below, the location of the catheter can be determined by viewing the pressure measured from the tip of the catheter. In the right atrium (RA), the pressure typically averages <5 mmHg and fluctuates a few mmHg. When the catheter is advanced into the right ventricle (RV), the systolic pressure increases to ~25 mmHg and the diastolic pressure remains similar to right atrial diastolic pressure. When the catheter enters the pulmonary artery (PA), the systolic pressure normally is similar to the right ventricular systolic pressure, but the diastolic pressure increases to about 10 mmHg because of pulmonic valve closure at the beginning of diastole. Just behind the tip of the catheter is a small balloon that can be inflated with air (~1 cc). When properly positioned in a branch of the pulmonary artery, the distal port measures pulmonary artery pressure (~ 25/10 mmHg; systolic/diastolic pressure). The balloon is then inflated, which occludes the branch of the pulmonary artery. When this occurs, the pressure in the distal port rapidly falls, and after several seconds, reaches a stable lower value that is very similar to left atrial pressure (mean pressure normally 8-10 mmHg). The pressure recorded during balloon inflation approximates left atrial pressure because the occluded vessel and its distal branches that eventually form the pulmonary veins act as an extension of the catheter. The pressure fluctuates during the cardiac cycle and normally shows a, c and v waves similar to the right atrial pressure tracing. The balloon is then deflated. This same catheter can be used to measure cardiac output by the thermodilution technique.
Why is PCWP measured?
It is helpful to measure PCWP to diagnose the severity of left ventricular failure and to quantify the degree of mitral valve stenosis. Both conditions elevate LAP and, therefore, PCWP. Aortic valve stenosis and regurgitation, and mitral regurgitation also elevate LAP. When these pressures are above 20 mmHg, pulmonary edema is likely to occur, which is a life-threatening condition. Note that LAP is the outflow or venous pressure for the pulmonary circulation and therefore increases in LAP are transmitted almost fully back to the pulmonary capillaries, increasing their hydrostatic pressure and filtration of fluid. By measuring PCWP, the physician can titrate the dose of diuretic drugs and other drugs that are used to reduce pulmonary venous and capillary pressure, and reduce pulmonary edema. Therefore, measurement of PCWP can help guide therapeutic efficacy.
PCWP is also important to measure when evaluating pulmonary hypertension. Pulmonary hypertension is often caused by increased pulmonary vascular resistance. To calculate this, pulmonary blood flow (usually measured by the thermodilution technique), pulmonary artery pressure and pulmonary venous pressure (PCWP) measurements are required. Pulmonary hypertension can also result from increases in pulmonary venous pressure and pulmonary blood volume secondary to left ventricular failure or mitral or aortic valve disease.
PCWP is also useful in evaluating blood volume status when fluids are administered during hypotensive shock. One practice is to administer fluids at a rate that maintains PCWP between 12-14 mmHg.
Revised 10/27/2023

 Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021)
Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021) Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)
Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)