Heart Failure - Introduction
What is heart failure?
Heart failure is the inability of the heart to supply adequate blood flow and, therefore, oxygen delivery to peripheral tissues and organs. Under perfusion of organs leads to reduced exercise capacity, fatigue, and shortness of breath. It can also lead to organ dysfunction (e.g., renal failure) in some patients.
What is the incidence of heart failure and its prognosis?
The American Heart Association estimates that over 6 million Americans currently have heart failure. Heart failure is the leading cause of hospitalization of patients over 65 years of age.
Despite many new advances in drug therapy and cardiac assist devices, the prognosis for chronic heart failure remains poor. One year mortality figures are 50-60% for patients diagnosed with severe failure, 15-30% in mild-to-moderate failure, and approximately 10% in mild or asymptomatic failure.
What are the causes of heart failure?
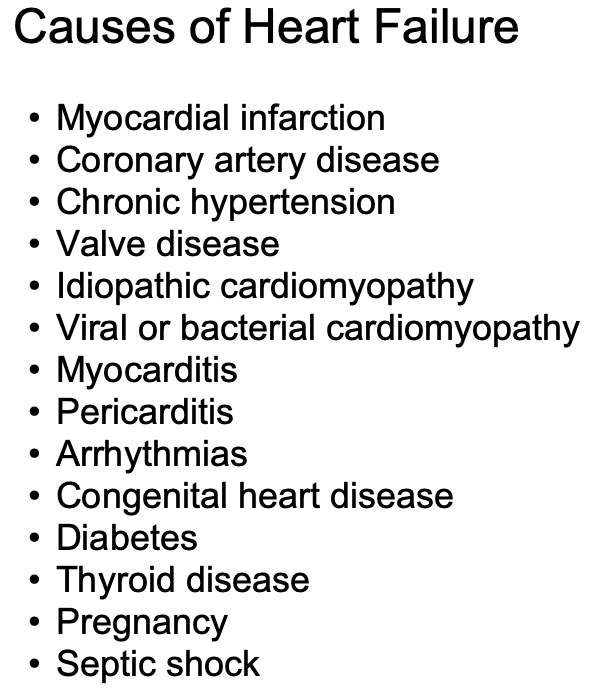 Heart failure is a clinical syndrome caused by disease or other abnormal conditions in the body. Factors originating from within the heart (i.e., intrinsic disease or pathology) or from external factors that place excessive demands upon the heart can cause heart failure. Intrinsic disease includes conditions such as dilated cardiomyopathy and hypertrophic cardiomyopathy. External factors that can lead to heart failure include long-term, uncontrolled hypertension, increased stroke volume (caused by increased blood volume or arterial-venous shunts), and hormonal disorders (e.g., hyperthyroidism).
Heart failure is a clinical syndrome caused by disease or other abnormal conditions in the body. Factors originating from within the heart (i.e., intrinsic disease or pathology) or from external factors that place excessive demands upon the heart can cause heart failure. Intrinsic disease includes conditions such as dilated cardiomyopathy and hypertrophic cardiomyopathy. External factors that can lead to heart failure include long-term, uncontrolled hypertension, increased stroke volume (caused by increased blood volume or arterial-venous shunts), and hormonal disorders (e.g., hyperthyroidism).
Acute heart failure develops rapidly and can be immediately life-threatening because the heart does not have time to undergo compensatory adaptations. Acute failure (hours/days) may result from cardiopulmonary by-pass surgery, acute infection (sepsis), acute myocardial infarction, valve dysfunction, severe arrhythmias, etc. Acute heart failure can be treated by correcting an underlying condition, or by pharmacological or surgical interventions.
Chronic heart failure is a long-term condition (months/years) that is associated with the heart undergoing adaptive responses (e.g., dilation, hypertrophy) to a precipitating cause. These adaptive responses, however, can be deleterious in the long-term and lead to a worsening condition.
The number one cause of heart failure is coronary artery disease (CAD). CAD reduces coronary blood flow and oxygen delivery to the myocardium. This leads to myocardial hypoxia and impaired function. Another common cause of heart failure is myocardial infarction, which is the final and sometimes fatal culmination of CAD. Infarcted tissue does not contribute to the generation of mechanical activity, so overall cardiac performance is diminished. Non-infarcted regions must compensate for the loss of function in the ischemic regions, and this extra burden can precipitate changes that lead to failure. Valvular disease and congenital defects place increased demands upon the heart that can precipitate failure. Cardiomyopathies of known origin (e.g., bacterial or viral) or idiopathic (unknown origin), can lead to failure. Myocarditis can have a similar effect. Arrhythmias, such as severe bradycardia or tachycardia, can also precipitate failure.
Go to: Pathophysiology of Heart Failure
Revised 11/05/2023

 Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021)
Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021) Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)
Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)