Venous Return - Hemodynamics
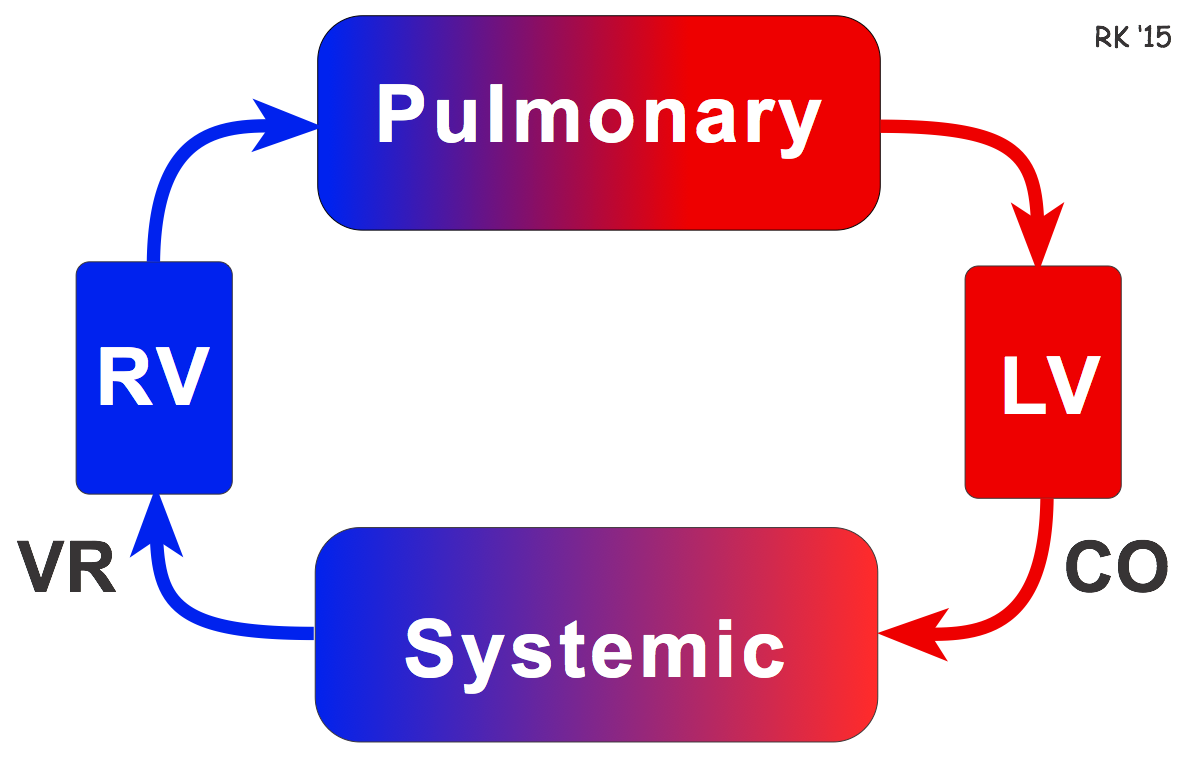 Venous return (VR) is the flow of blood back to the heart. Under steady-state conditions, venous return must equal cardiac output (CO) when averaged over time because the cardiovascular system is essentially a closed loop (see figure). Otherwise, blood would accumulate in either the systemic or pulmonary circulations. Although cardiac output and venous return are interdependent, each can be independently regulated.
Venous return (VR) is the flow of blood back to the heart. Under steady-state conditions, venous return must equal cardiac output (CO) when averaged over time because the cardiovascular system is essentially a closed loop (see figure). Otherwise, blood would accumulate in either the systemic or pulmonary circulations. Although cardiac output and venous return are interdependent, each can be independently regulated.
The circulatory system comprises two circulations (pulmonary and systemic) in series between the right ventricle (RV) and the left ventricle (LV) as depicted in the figure. Balance is achieved by the Frank-Starling mechanism. For example, if systemic venous return is suddenly increased (e.g., changing from upright to supine position), right ventricular preload increases, leading to an increase in stroke volume and pulmonary blood flow. Increased pulmonary venous return to the left atrium leads to increased filling (preload) of the left ventricle, which increases left ventricular stroke volume by the Frank-Starling mechanism. In this way, an increase in venous return to the heart leads to an equivalent increase in cardiac output.
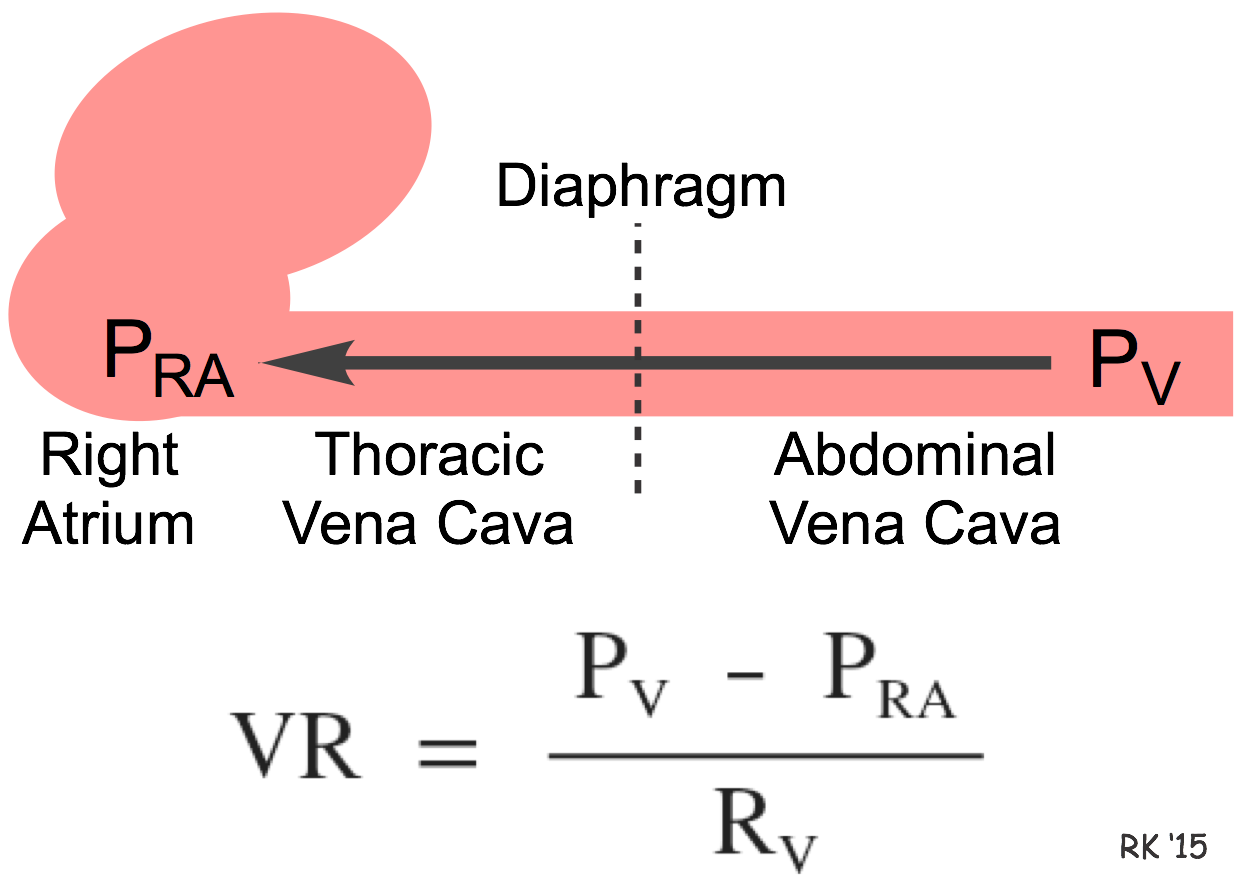 Hemodynamically, venous return (VR) to the heart from the venous vascular beds is determined by a pressure gradient (venous pressure, PV, minus right atrial pressure, PRA) divided by the venous vascular resistance (RV) between the two pressures as shown in the figure. Therefore, increased venous pressure or decreased right atrial pressure, or decreased venous resistance leads to an increase in venous return. PRA is normally very low (fluctuating a few mmHg around a mean of 0 mmHg) and PV in peripheral veins (when the body is supine) is only a few mmHg higher. Therefore, the pressure gradient driving venous return from peripheral veins to the heart is relatively low (<10 mmHg). Because of this, small changes of only a few mmHg in either PV or PRA can cause a large percent change in the pressure gradient, and therefore significantly alter the return of blood to the right atrium. For example, during lung expansion (inspiration), PRA can transiently fall by several mmHg, while the PV in the abdominal compartment may increase by a few mmHg. These changes result in a large increase in the pressure gradient driving venous return from the peripheral circulation to the right atrium.
Hemodynamically, venous return (VR) to the heart from the venous vascular beds is determined by a pressure gradient (venous pressure, PV, minus right atrial pressure, PRA) divided by the venous vascular resistance (RV) between the two pressures as shown in the figure. Therefore, increased venous pressure or decreased right atrial pressure, or decreased venous resistance leads to an increase in venous return. PRA is normally very low (fluctuating a few mmHg around a mean of 0 mmHg) and PV in peripheral veins (when the body is supine) is only a few mmHg higher. Therefore, the pressure gradient driving venous return from peripheral veins to the heart is relatively low (<10 mmHg). Because of this, small changes of only a few mmHg in either PV or PRA can cause a large percent change in the pressure gradient, and therefore significantly alter the return of blood to the right atrium. For example, during lung expansion (inspiration), PRA can transiently fall by several mmHg, while the PV in the abdominal compartment may increase by a few mmHg. These changes result in a large increase in the pressure gradient driving venous return from the peripheral circulation to the right atrium.
Although the above relationship is true for the hemodynamic factors that determine the flow of blood from peripheral veins (abdominal venous cava in the figure) back to the right atrium of the heart, it is important not to lose sight of the fact that blood flowing through the entire systemic circulation can be represented by either the cardiac output or the venous return because these are equal in the steady-state owing to the circulatory system being closed. Therefore, one could just as well say that venous return is determined by the mean aortic pressure minus the mean right atrial pressure, divided by the resistance of the entire systemic circulation (i.e., the systemic vascular resistance) because this determines the flow of blood throughout the entire systemic circulation, which returns to the heart.
There is much confusion about the pressure gradient that determines venous return, largely because of different conceptual models that have been used to describe venous return. Although transient differences occur between the flow of blood leaving the heart (cardiac output) and entering the heart (venous return), these differences when they occur cause adjustments that rapidly lead to a new steady-state in which cardiac output (flow out) equals venous return (flow in).
Transient changes in venous return can occur in response to several factors, as listed below:
- Muscle contraction. Rhythmical contraction of limb muscles occurring during normal locomotory activity (e.g., walking, running) promotes venous return by the muscle pump mechanism.
- Decreased venous compliance. Sympathetic activation of veins decreases venous compliance, increases central venous pressure and promotes venous return indirectly by augmenting cardiac output through the Frank-Starling mechanism, which increases the total blood flow through the circulatory system.
- Respiratory activity. During respiratory inspiration, the venous return transiently increases because of a decrease in right atrial pressure. The opposite occurs during expiration.
- Vena cava compression. An increase in the resistance of the vena cava, as occurs when the thoracic vena cava becomes compressed during a Valsalva maneuver or during late pregnancy, decreases venous return.
- Gravity. The effects of gravity on venous return seem paradoxical because when a person stands up hydrostatic forces cause the right atrial pressure to decrease and the venous pressure in the dependent limbs to increase. This increases the pressure gradient for venous return from the dependent limbs to the right atrium; however, venous return paradoxically decreases. The reason for this is when a person initially stands and before the baroreceptor reflex is activated, cardiac output and arterial pressure decrease because right atrial pressure and ventricular preload falls, which decreases stroke volume and cardiac output by the Frank-Starling mechanism. The flow through the entire systemic circulation falls because arterial pressure falls more than right atrial pressure; therefore, the pressure gradient driving flow throughout the entire circulatory system is decreased.
Revised 01/24/2023

 Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021)
Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021) Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)
Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)