Cardiac Preload
Preload can be defined as the initial stretching of the cardiac myocytes before contraction. Preload, therefore, is related to muscle sarcomere length. Because sarcomere length cannot be determined in the intact heart, other indices of preload are used, such as ventricular end-diastolic volume or pressure.
When venous return to the heart is increased, the end-diastolic pressure and volume of the ventricles are increased, which stretches the sarcomeres, increasing their preload. In contrast, hypovolemia resulting from a loss of blood volume (e.g., hemorrhage) leads to less ventricular filling and therefore shorter sarcomere lengths (reduced preload). Changes in ventricular preload dramatically affect ventricular stroke volume by what is called the Frank-Starling mechanism. Increased preload increases stroke volume, whereas decreased preload decreases stroke volume by altering the force of contraction of the cardiac muscle.
The concept of preload can apply to either the ventricles or atria. Regardless of the chamber, the preload is related to the chamber volume, and therefore sarcomere length, just before contraction.
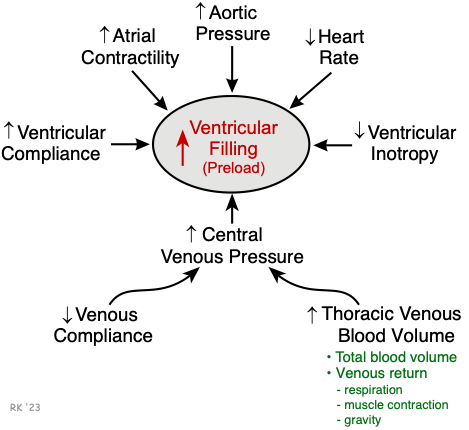 Ventricular filling and therefore preload is increased by:
Ventricular filling and therefore preload is increased by:
- Increased central venous pressure that can result from decreased venous compliance (e.g., caused by sympathetic activation of venous smooth muscle) or increased thoracic blood volume. The latter can be increased by either increased total blood volume or by venous return augmented by increased respiratory activity, increased skeletal muscle pump activity, or by effects of gravity (e.g., head-down tilt).
- Increased ventricular compliance, which results in a greater expansion of the chamber during filling at a given filling pressure.
- Increased atrial force of contraction resulting from sympathetic stimulation of the atria or from increased filling of the atria and therefore increased atrial contractile force through the Frank-Starling mechanism.
- Increased aortic pressure, which increases the afterload on the ventricle, reduces stroke volume by increasing end-systolic volume, and leads to a secondary increase in ventricular preload.
- Reduced heart rate, which increases ventricular filling time.
- Reduced ventricular inotropy leads to a compensatory increase in ventricular preload.
- Pathological conditions, such as valve defects (e.g., valve stenosis and insufficiency) also alter ventricular preload.
Ventricular preload is decreased by:
- Decreased venous blood pressure, most commonly resulting from reduced blood volume (e.g., hemorrhage) or gravity, causing blood to pool in the lower limbs when standing upright.
- Impaired atrial contraction that can result from atrial arrhythmias, such as atrial fibrillation.
- Increased heart rate (e.g., atrial tachycardia), which reduces ventricular filling time.
- Decreased ventricular afterload, which enhances forward flow (i.e., ejection) reducing end-systolic volume and end-diastolic volume secondarily.
- Ventricular diastolic failure (decreased ventricular compliance) caused, for example, by ventricular hypertrophy or impaired relaxation.
- Inflow (mitral and tricuspid) valve stenosis, which reduces ventricular filling.
Revised 01/22/2023

 Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021)
Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021) Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)
Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)