Adrenergic and Cholinergic Receptors in Blood Vessels
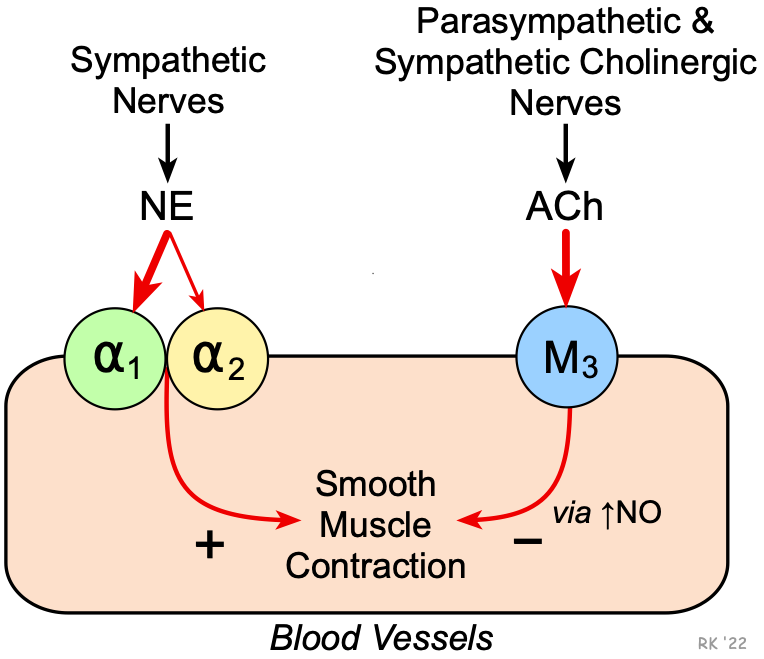 Most arteries and veins in the body are innervated by sympathetic adrenergic nerves, which release norepinephrine (NE) as a neurotransmitter. Some blood vessels are innervated by parasympathetic cholinergic or sympathetic cholinergic nerves, both of which release acetylcholine (ACh) as their primary neurotransmitter. Neurotransmitter binding to the adrenergic and cholinergic receptors activate signal transduction pathways that cause the observed changes in vascular function.
Most arteries and veins in the body are innervated by sympathetic adrenergic nerves, which release norepinephrine (NE) as a neurotransmitter. Some blood vessels are innervated by parasympathetic cholinergic or sympathetic cholinergic nerves, both of which release acetylcholine (ACh) as their primary neurotransmitter. Neurotransmitter binding to the adrenergic and cholinergic receptors activate signal transduction pathways that cause the observed changes in vascular function.
NE preferentially binds α1-adrenoceptors to cause smooth muscle contraction and vasoconstriction. Similar responses occur when NE binds to postjunctional α2-adrenoceptors on some blood vessels. NE also binds weakly to postjunctional β2-adrenoceptors, which causes vasodilation (this can be observed during alpha adrenoceptor blockade), although this vasodilator effect of NE is relatively minor and overwhelmed by alpha adrenoceptor-mediated vasoconstriction. Circulating epinephrine (EPI) binds with high affinity to smooth muscle β2-adrenoceptors to cause vasodilation in some organs; however, the effect of EPI is very concentration-dependent. While EPI has a higher affinity for β2 than postjunctional α1 or α2-adrenoceptors, at high concentrations it does bind to the postjunctional α1 and α2-adrenoceptors, which can override the vasodilatory effects of β2-adrenoceptor stimulation and produce vasoconstriction.
Some blood vessels in the body (e.g., coronary vessels) are innervated by parasympathetic cholinergic fibers. These nerves release ACh, which binds to muscarinic M3 receptors on the smooth muscle and/or endothelium that are linked to Gq-proteins. It has been shown that endothelial M3 receptors also stimulate the formation of nitric oxide (NO), which causes smooth muscle relaxation. Note, however, that in the absence of NO, ACh causes smooth muscle contraction through smooth muscle M3 receptors. This latter finding has been used to assess coronary vascular dysfunction in humans, in which NO production is diminished in diseased coronary arteries. In contrast to other arteries, cerebral arteries appear to have M5 muscarinic receptors that produce vasodilation in response to ACh.
Some arterial blood vessels in skeletal muscle of dogs and cats (but not humans) are innervated by sympathetic cholinergic nerves that release ACh and cause vasodilation. In species having sympathetic cholinergic nerves, their activation may contribute to active hyperemia in skeletal muscle, particularly at the onset of exercise. Sympathetic cholinergic nerves controlled by hypothalamic thermoregulatory nuclei play an important role in producing cutaneous active vasodilation when skin and body core temperature increase in warm environments.
Drugs are available for blocking vascular adrenergic receptors. Alpha-blockers, for example, are used in treating hypertension. Some of the alpha-blockers are relatively selective for a specific receptor subtype, whereas others as non-selective. Drugs such as atropine block muscarinic receptors.
Revised 12/9/2022

 Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021)
Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021) Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)
Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)