Adrenergic and Cholinergic Receptors in the Heart
Sympathetic adrenergic nerves innervate the SA and AV nodes, conduction pathways, and myocytes in the heart. These adrenergic nerves release the neurotransmitter norepinephrine (NE), which binds to specific receptors in the target tissue to produce their physiological responses. Neurotransmitter binding to receptors activates signal transduction pathways that cause the observed changes in cardiac function.
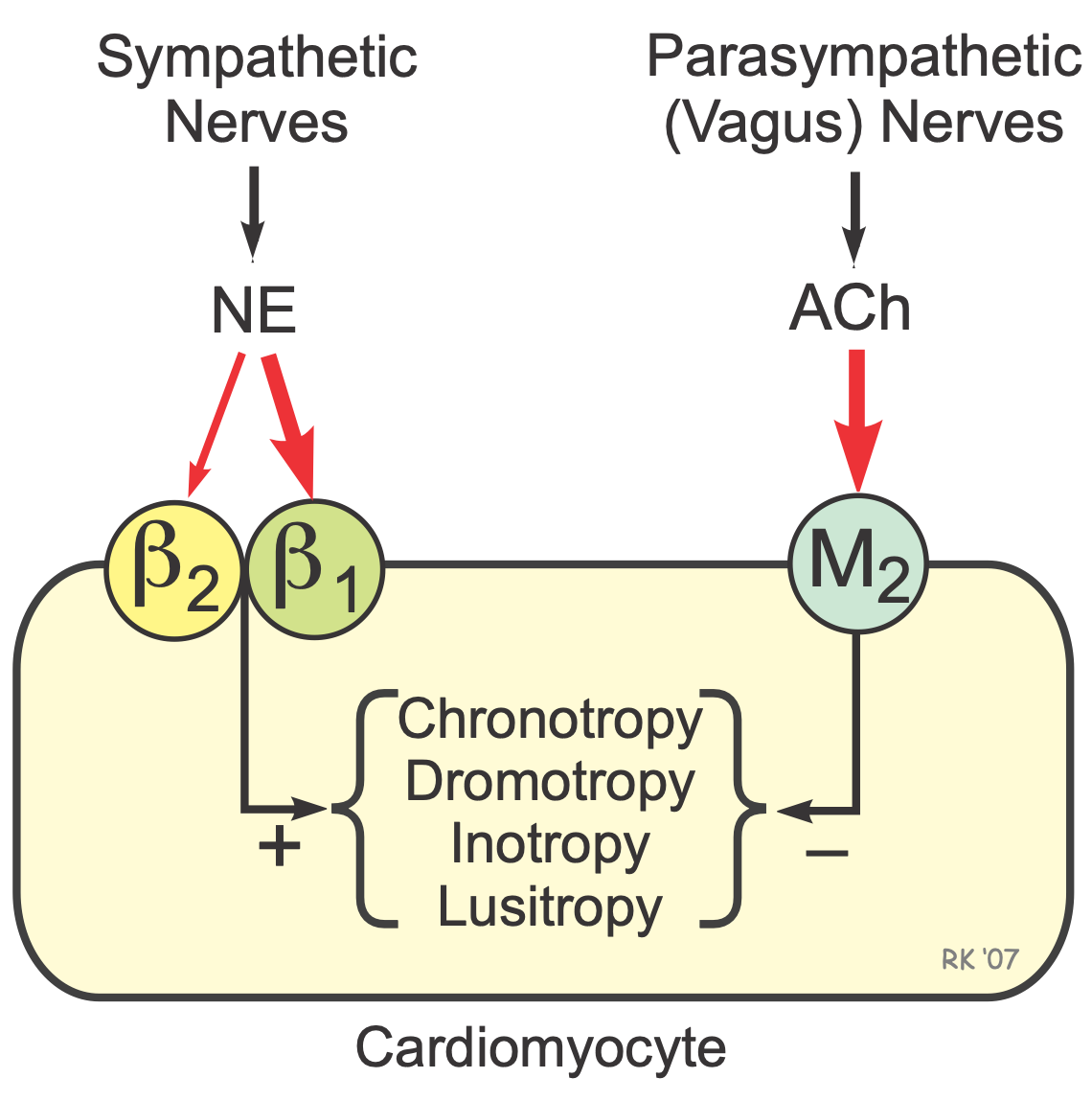 Adrenergic receptors (adrenoceptors) are receptors that bind adrenergic agonists such as the sympathetic neurotransmitter NE and the circulating hormone epinephrine (EPI). The most important adrenoceptor in the heart (not including coronary vascular adrenoceptors) is the β1-adrenoceptor. When activated by a β1-agonist such as NE or EPI, heart rate is increased (positive chronotropy), conduction velocity is increased (positive dromotropy), contractility is increased (positive inotropy), and the rate of myocyte relaxation is increased (positive lusitropy).
Adrenergic receptors (adrenoceptors) are receptors that bind adrenergic agonists such as the sympathetic neurotransmitter NE and the circulating hormone epinephrine (EPI). The most important adrenoceptor in the heart (not including coronary vascular adrenoceptors) is the β1-adrenoceptor. When activated by a β1-agonist such as NE or EPI, heart rate is increased (positive chronotropy), conduction velocity is increased (positive dromotropy), contractility is increased (positive inotropy), and the rate of myocyte relaxation is increased (positive lusitropy).
There are also β2-adrenoceptors in the heart, and stimulation by β2-agonists has similar cardiac effects as β1-adrenoceptor stimulation. The β2-adrenoceptors become functionally more important in heart failure because β1-adrenoceptors become down regulated.
NE can also bind to α1-adrenoceptors found on myocytes (not shown in figure) to produce small increases in inotropy. Circulating catecholamines (e.g., norepinephrine and epinephrine) released by the adrenal medulla also bind to these same alpha and beta adrenoceptors in the heart.
Besides sympathetic adrenergic nerves, the heart is innervated by parasympathetic cholinergic nerves derived from the vagus nerves. Acetylcholine (ACh) released by these nerves binds to M2 muscarinic receptors in the cardiac muscle, especially at the SA and AV nodes that have a large amount of vagal innervation. This produces negative chronotropy and dromotropy in the heart, as well as negative inotropy and lusitropy in the atria (the negative inotropic and lusitropic effects of vagal stimulation are relatively weak in the ventricles).
The autonomic nerve terminals also possess adrenergic and cholinergic receptors (prejunctional receptors) that function to regulate the release of NE (not shown in figure). Prejunctional α2-adrenoceptors inhibit NE release, whereas prejunctional β2-adrenoceptors facilitate NE release. Prejunctional M2 receptors inhibit NE release, which is one mechanism by which vagal stimulation overrides sympathetic stimulation in the heart.
Drugs are available for blocking adrenergic and cholinergic receptors. For example, beta-blockers are used in the treatment of angina, hypertension, arrhythmias, and heart failure. Muscarinic receptor blockers such as atropine are used to treat electrical disturbances (e.g., bradycardia and conduction blocks) associated with excessive vagal stimulation of the heart. Many of these adrenergic and cholinergic blockers are relatively selective for a specific receptor subtype.
Revised 12/9/2022

 Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021)
Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021) Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)
Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)