Abnormal Rhythms - Definitions
General Terms:
Normal sinus rhythm – heart rhythm controlled by sinus node at 60-100 beats/min; each P wave followed by QRS and each QRS preceded by a P wave.
Bradycardia – a heart rate that is lower than normal.
Tachycardia – a heart rate that is higher than normal.
Paroxysmal – an arrhythmia that suddenly begins and ends.
Specific Arrhythmias:
Sinus bradycardia – low sinus rate <60 beats/min.
Sinus tachycardia – high sinus rate of 100-180 beats/min as occurs during exercise or other conditions that lead to increased SA nodal firing rate.
Sick sinus syndrome – a disturbance of SA nodal function that results in a markedly variable rhythm (cycles of bradycardia and tachycardia).
Atrial tachycardia – a series of 3 or more consecutive atrial premature beats occurring at a frequency >100/min; usually because of abnormal focus within the atria and paroxysmal in nature, therefore the appearance of P wave is altered in different ECG leads. This type of rhythm includes paroxysmal atrial tachycardia (PAT).
Atrial flutter – sinus rate of 250-350 beats/min.
Atrial fibrillation – uncoordinated atrial depolarizations.
Junctional escape rhythm – SA node suppression can cause AV node-generated rhythm of 40-60 beats/min (not preceded by P wave).
AV nodal blocks – a conduction block within the AV node (or occasionally in the bundle of His) that impairs impulse conduction from the atria to the ventricles.
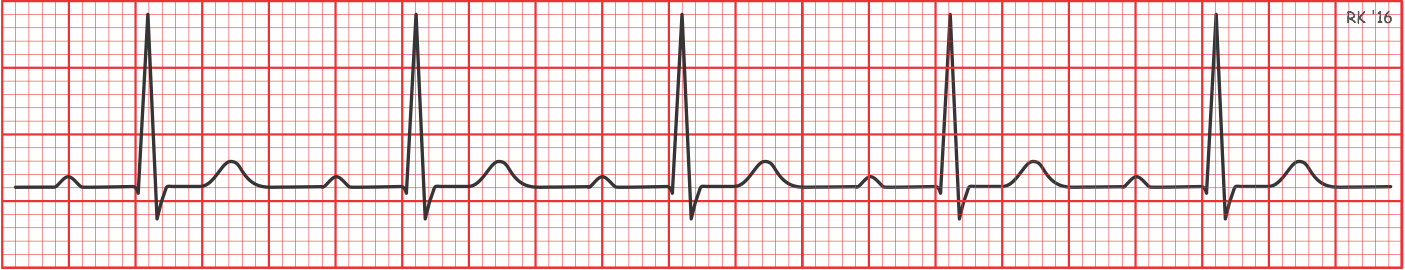
- First-degree AV nodal block – the conduction velocity is slowed so that the PR interval is increased to greater than 0.20 seconds. In the tracing below, the PR interval is 0.24 sec. The rate is not altered by the prolonged PR interval because it is still being controlled by the SA node. This type of block can be caused by enhanced vagal tone, digitalis, beta-blockers, calcium channel blockers, or ischemic damage to the nodal tissue.
- Second-degree AV nodal block – the conduction velocity is slowed to where some impulses from the atria cannot pass through the AV node. This results in P waves that are not followed by QRS complexes. There are two subtypes of second-degree AV blocks: Mobitz Type I and Mobitz Type II.
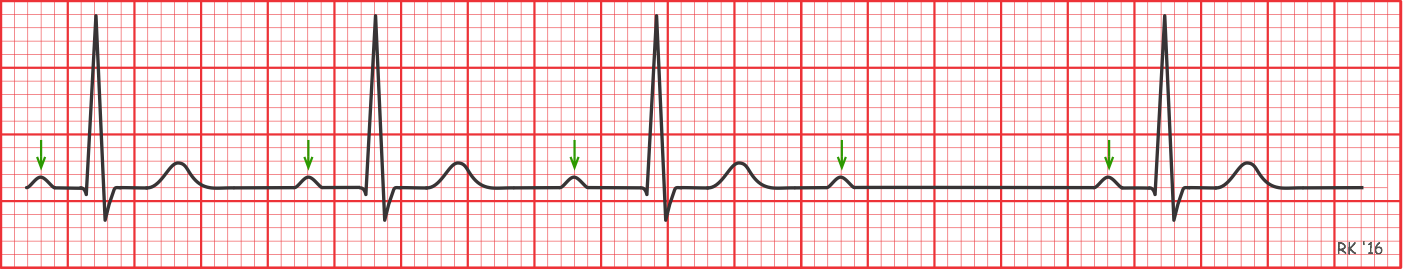
- Mobitz I (also called “Wenckebach”) is a condition where the PR interval gradually increases over several beats until it is sufficiently prolonged (that is, AV conduction is sufficiently impaired) that the impulse cannot pass into the ventricles (i.e., a QRS will not follow the P wave). In the first tracing below, the PR interval for the first beat is 0.16 sec and increases to 0.24 sec by the third beat. In the fourth beat, the P wave is not followed by a QRS; therefore, the ventricular beat is dropped. The fifth beat starts this cycle over again.
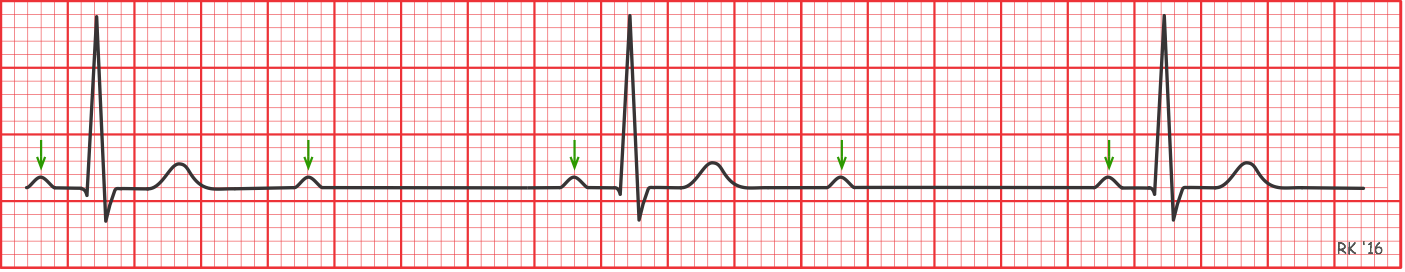
- Mobitz II occurs is when the P-R interval is fixed in duration, but some P waves are not followed by a QRS, as illustrated in the second tracing below. This is an example of a 2:1 rhythm because there are two P waves for each QRS. Other ratios (e.g., 3:2) may occur. In either type of second-degree block, the ventricular rate will be less than the normal sinus rhythm (indicated by green arrows in figures). Also note that the QRS complexes appear normal in shape and duration because they are still being triggered by impulses from the atria passing through the AV node.
- Mobitz I (also called “Wenckebach”) is a condition where the PR interval gradually increases over several beats until it is sufficiently prolonged (that is, AV conduction is sufficiently impaired) that the impulse cannot pass into the ventricles (i.e., a QRS will not follow the P wave). In the first tracing below, the PR interval for the first beat is 0.16 sec and increases to 0.24 sec by the third beat. In the fourth beat, the P wave is not followed by a QRS; therefore, the ventricular beat is dropped. The fifth beat starts this cycle over again.
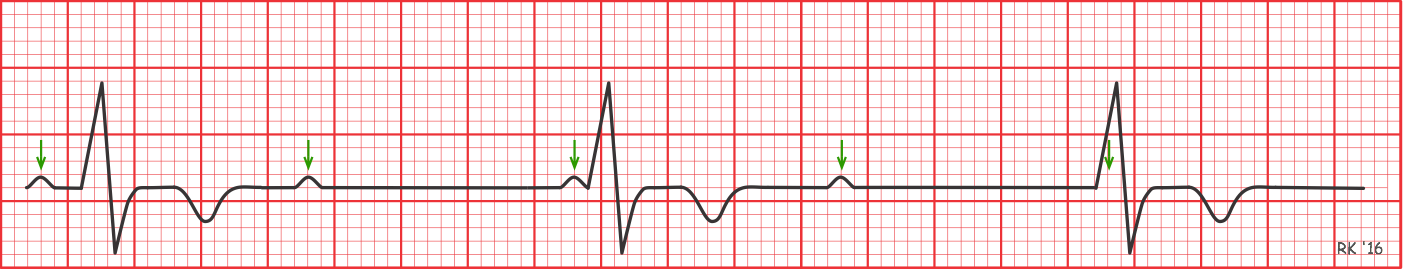
- Third-degree AV nodal block – conduction through the AV node is completely blocked so that no impulses can be transmitted from the atria to the ventricles. QRS complexes still occur (escape rhythm), but they originate from within the AV node, bundle of His, or other ventricular regions. Therefore, QRS complexes will not be preceded by P waves. There will be complete asynchrony between the P wave and QRS complexes. Atrial rate and rhythm may be completely normal (green arrows indicate P waves, although in the last beat it is obscured by the QRS), but ventricular rate will be reduced, the extent of which depends on the location of the site generating the ventricular rhythm. Ventricular rates typically range from 30 to 40 beats/min if the ventricular foci generating ventricular rhythm are below the bundle of His. The following figure shows QRS complexes having an abnormal shape and prolonged duration because ventricular depolarization does not follow normal conduction pathways.
Supraventricular tachycardia (SVT) – usually caused by reentry currents within the atria or between ventricles and atria producing high heart rates of 140-250; the QRS complex is usually normal width, unless there are also intraventricular conduction blocks (e.g., bundle branch block).
Ventricular premature beats (VPBs) – caused by ectopic ventricular foci; characterized by widened QRS; often referred to as a premature ventricular complex, or PVC. Note the wide and abnormally shaped QRS that is generated prematurely in the following ECG rhythm strip: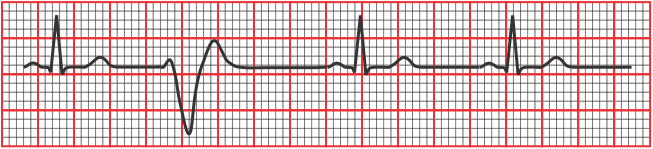
Ventricular tachycardia (VT) – high ventricular rate caused by aberrant ventricular automaticity (ventricular foci) or by intraventricular reentry can be sustained or nonsustained (paroxysmal). They are typically characterized by widened QRS (>0.14 sec); rates of 100 to 280 beats/min; life-threatening.
Ventricular flutter – very rapid ventricular depolarizations >250/min; sine wave appearance; leads to fibrillation.
Ventricular fibrillation – uncoordinated ventricular depolarizations; leads to death if not quickly converted to a normal rhythm or at least a rhythm compatible with life.
For information on the pharmacologic treatment of arrhythmias, go to: cvpharmacology.com/antiarrhy/antiarrhythmic.
Revised 11/01/2023

 Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021)
Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021) Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)
Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)