Altered Impulse Conduction
Abnormal conduction of impulses within the heart can lead to arrhythmias. The most common cause of abnormal conduction is localized or regional depolarization because of hypoxia caused by impaired coronary blood flow. Depolarization decreases the action potential amplitude and rate of depolarization (phase 0 slope is decreased), both of which decrease the velocity of action potential conduction or completely stop the conduction of action potentials (i.e., conduction block). Conduction blocks can also be caused at the AV node by excessive vagal activation or because of drugs that reduce conduction, such as beta-blockers and calcium-channel blockers.
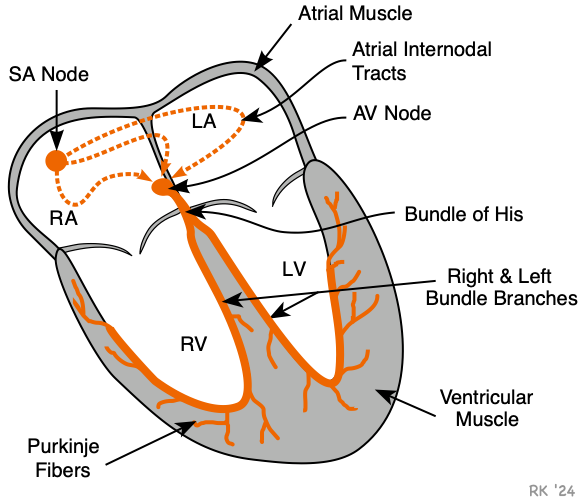 Conduction blocks can occur at the AV node, bundle of His, or bundle branches as shown in the figure. There are three categories of conduction blocks: AV block, bundle branch block, and hemiblock. When there is an AV block, impulses originating in the SA node cannot enter the ventricles. This type of block can occur either at the AV node, at the common bundle of His, or when both bundle branches are blocked. When this occurs, a pacemaker site distal to the block will become the new pacemaker for the ventricles. These secondary pacemaker sites have an intrinsic rate (30-50 impulses/min, depending on the site), which is considerably slower than the SA node. Therefore, an AV conduction block will lead to ventricular bradycardia. When either the left or right bundle branch is blocked (bundle branch block), impulses still travel from the atria to the ventricles, so there is no complete block and the ventricles will still be driven by the SA node. However, the sequence and timing of ventricular depolarization will be altered (see below). A hemiblock occurs when the left anterior or posterior fascicle of the left bundle branch becomes blocked.
Conduction blocks can occur at the AV node, bundle of His, or bundle branches as shown in the figure. There are three categories of conduction blocks: AV block, bundle branch block, and hemiblock. When there is an AV block, impulses originating in the SA node cannot enter the ventricles. This type of block can occur either at the AV node, at the common bundle of His, or when both bundle branches are blocked. When this occurs, a pacemaker site distal to the block will become the new pacemaker for the ventricles. These secondary pacemaker sites have an intrinsic rate (30-50 impulses/min, depending on the site), which is considerably slower than the SA node. Therefore, an AV conduction block will lead to ventricular bradycardia. When either the left or right bundle branch is blocked (bundle branch block), impulses still travel from the atria to the ventricles, so there is no complete block and the ventricles will still be driven by the SA node. However, the sequence and timing of ventricular depolarization will be altered (see below). A hemiblock occurs when the left anterior or posterior fascicle of the left bundle branch becomes blocked.
When the conduction block is not a complete AV block (e.g., as occurs with left bundle branch block), electrical impulses can travel along alternate conduction pathways to depolarize the ventricles. When this occurs, it takes longer for the ventricles to depolarize. This is manifested as an increase in the duration of the QRS complex, and a change in its shape. Occasionally, the abnormal conduction pathways can cause a self-perpetuating, circular movement of electrical activation. This is termed reentry and is a major cause of ventricular and supraventricular tachycardias.
Revised 10/27/2023

 Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021)
Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021) Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)
Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)