Altered Impulse Formation
Abnormal Impulses
The normal pacemaker site for the heart is within the SA node. Cells within this pacemaker region have an intrinsic firing rate that is modulated primarily by changes in autonomic nerve activity. If there is a high level of vagal tone on the SA node, then this will cause sinus bradycardia (a sinus rate <60 beats/min). Conversely, an abnormally high level of sympathetic tone on the SA node will cause sinus tachycardia (a sinus rate >100 beats/min). In a condition called sick sinus syndrome, the SA nodal firing rate alternates between bradycardia and normal rhythm.
Abnormal impulse formation can be caused by the expression of ectopic pacemaker sites within the heart. These are sites outside the SA node that can spontaneously depolarize and thereby produce atrial or ventricular action potentials independent of SA nodal firing. This can occur when the SA node ceases to operate as the dominant pacemaker site (e.g., when the SA node is damaged), or in the presence of normal SA nodal function. One mechanism by which this can occur is the transformation of normal, non-pacemaker action potentials (e.g., in Purkinje cells or myocytes) into pacemaker action potentials. This can occur when a cell becomes hypoxic, which leads to membrane depolarization. As a cell becomes progressively depolarized from -90 mV to -50 mV, fast Na+ channels become progressively inactivated. Inactivated Na+ channels cannot open and participate in the initial depolarization (phase 0) of the action potential. At a membrane potential of about –50 mV, all the fast Na+ channels are inactivated. When this occurs, action potentials can still be elicited; however, the inward current is carried by Ca++ (slow inward channels) exclusively. These action potentials resemble those found in pacemaker cells of the SA node, and sometimes display spontaneous depolarization and automaticity. This mechanism may serve as the electrophysiological mechanism behind certain types of ectopic beats and arrhythmias, particularly in ischemic heart disease and following myocardial infarction.
Triggered Activity
Triggered activity occurs when abnormal action potentials are triggered by a preceding action potential and can cause either atrial or ventricular tachycardia. The abnormal impulses are spontaneous (yet triggered) depolarizations that occur during either phase 3 or 4 of an action potential (called “afterdepolarizations”). Triggered activity is more likely to occur when the action potential duration is abnormally long. This can occur in some patients having a genetic defect that produces prolonged action potentials, manifested as a long Q-T interval on the electrocardiogram (long Q-T syndrome). Drugs that prolong the action potential duration, such as potassium-channel blockers (Class III antiarrhythmics), can sometimes precipitate triggered activity.
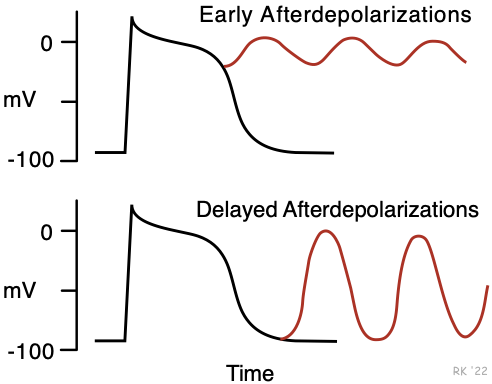 Afterdepolarizations can be early or delayed. Early afterdepolarizations occur during late phase 2 or phase 3 and can lead to a salvo of several rapid action potentials or a prolonged series of action potentials. This form of triggered activity is more likely to occur when the action potential duration is increased. Therefore, drugs that decrease action potential duration (e.g., lidocaine) are often effective against tachyarrhythmias generated by this mechanism. Calcium channel blockers, by decreasing gCa++, can also be effective in their treatment.
Afterdepolarizations can be early or delayed. Early afterdepolarizations occur during late phase 2 or phase 3 and can lead to a salvo of several rapid action potentials or a prolonged series of action potentials. This form of triggered activity is more likely to occur when the action potential duration is increased. Therefore, drugs that decrease action potential duration (e.g., lidocaine) are often effective against tachyarrhythmias generated by this mechanism. Calcium channel blockers, by decreasing gCa++, can also be effective in their treatment.
Delayed afterdepolarizations occur in late phase 3 or early phase 4 when the action potential is nearly or fully repolarized. The mechanism is poorly understood; however, this type of arrhythmia is found to be associated with high intracellular Ca++ concentrations, as occurs with digitalis toxicity or excessive catecholamine stimulation. The triggered impulse can lead to a series of rapid depolarizations (i.e., a tachyarrhythmia).
Revised 10/27/2023

 Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021)
Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021) Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)
Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)